
When “More” Doesn’t Mean “Moderate”
When “More” Doesn’t Mean “Moderate” Understanding the Acute Problem Riddle in MDM. Let’s be honest — it makes sense to assume that if a patient
The arrival of artificial intelligence (AI) in healthcare raises pressing questions about the future of the healthcare workforce, professional guilds, and industry-wide best-practice. What lessons can we glean from history to better understand the opportunities and risks? The Luddites, Nurse Practitioners (NPs), and driverless cars offer compelling case studies that reveal how technology and societal change disrupt professions and create new opportunities.
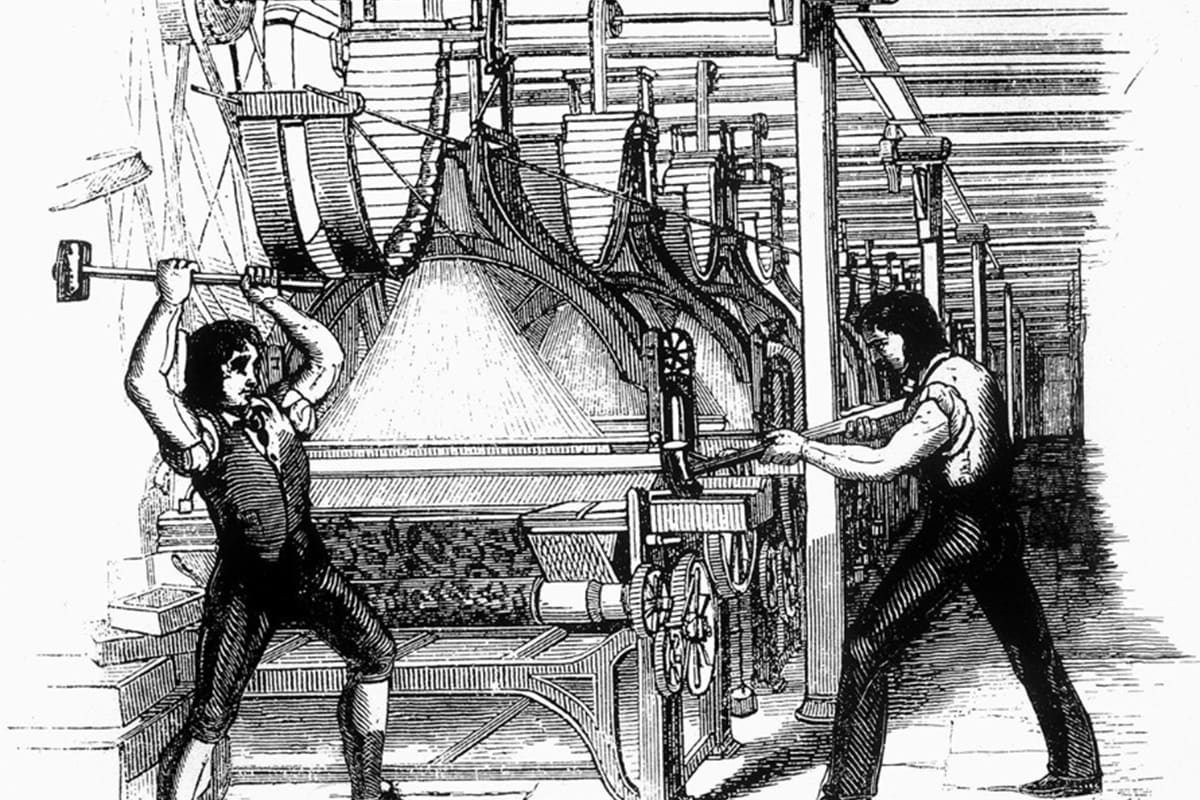
The Luddites of the early 19th century were highly skilled artisans whose livelihoods were directly threatened by automated machinery. Technological advancements allowed for the faster and cheaper production of goods, particularly textiles. Their protests exposed the tension between technological progress and its social costs, leading to severe repercussions, including “machine breaking” being declared a capital crime in England. The plight of the Luddites underscores a critical challenge for today’s leaders: managing the disruptive potential of automation without fracturing societal cohesion.
The Luddites also presented a precinct argument for healthcare; they made a strong case for the superior quality and durability of hand made goods relative to the machine produced counterparts. They argued slower hand-made production processes reduced replacement costs, and that the transferability of technology relative to the tribal knowledge of weavers opened the door to foreign production further weakening the demand for domestic products.
The evolution of the NP role in the United States provides a modern counterpoint with an entirely different outcome. Empowered by education, credentialing, and decision-support technologies, NPs have expanded their scope of practice to include diagnosing, prescribing, and treating patients—work not so long ago reserved exclusively for physicians. While their training is less time extensive than that of Medical Doctors (MDs), NPs have proven essential in addressing gaps in care and improving patient access, particularly in underserved areas.
This shift in scope demonstrates how technological and administrative change can empower a broader range of professionals to take on higher-value decision making roles, provided they are equipped with the right tools and support systems. For healthcare executives, this offers insight for integrating AI to augment human expertise without overwriting the unique contributions of cognition in care delivery. Healthcare institutions have the opportunity to provide the job description of ‘knowledge worker’ to a larger share of medical professionals and healthcare administrators by focusing on AI applications that extend decision making capabilities to workers performing rote manual or computer tasks.
Cruise was an American self-driving car company founded in 2011 in San Francisco, CA. After demonstrating a successful prototype and a unique go to market strategy, Cruise was acquired by General Motors in 2016 to jump-start the legacy automaker’s access to AI innovation and provide a direct stake in bringing autonomously powered vehicles to the American market.
In August 2023, Cruise received a permit from the state of California to operate a fleet of driverless taxis. In October 2023 the license was immediately suspended after a Cruise taxi struck a pedestrian in San Francisco who became lodged in the undercarriage. The driverless car failed to stop, and the pedestrian was killed. The U.S. Department of Justice and the U.S. Securities and Exchange Commission each opened investigations, and concluded insufficient leadership was the root cause of insufficient product quality control. GM ceased funding Cruise in December 2024, and restructuring of the LLC asset is expected to complete by mid-2025.
Like driverless cars, mistakes caused by AI in healthcare delivery represents a fatal flaw, immediately halting the progress of the corporate entity responsible for the mistake, and quite possibly eroding trust in the underlying technology itself. Change in healthcare must proceed in a highly disciplined manner, with carefully designed control trials to ensure the performance of these technologies exceeds expectations.
AI is poised to impact healthcare in ways that are both profound and nuanced. From summarizing complex, decentralized, and discordant medical information to supporting pattern recognition in diagnostics, and care model efficacy, the hope is this technology will increase healthcare providers’ ability to inductively reason, access highly specific expertise, and empathize.
As AI takes on increasingly sophisticated tasks, it implicitly challenges the traditional boundaries of healthcare roles. Consider these implications:
The challenge is not to position AI to maximally disrupt healthcare labor, but instead asking how to deploy it in a way that amplifies human decision making capability. Focusing solely on the replacement value of labor with AI fails to recognize the increasing complexity of public health decision making. Americans are very sick and getting sicker. Long-standing preventive care practices and novel therapeutics can be considered scarce resources that must be distributed efficiently and ethically. AI can better navigate complex data analysis and pattern recognition than human analysts. It can complete data transfer tasks and information synthesis and summarization in a fraction of the time of a human researcher. All of the time AI can save the system can translate directly to additional time and minds on the increasingly complex problems of extending our welfare. For healthcare leaders, this means asking:
One can hope that AI redefines healthcare labor markets in ways that mirror more closely the trajectory of NPs, rather than the Luddites, and without the collateral damage of autonomous vehicles. By expanding the scope of what professionals can achieve and creating pathways to decision-making roles, AI could unlock a new era of productivity and patient care innovation, and provide human guardrails against fatal flaws.

When “More” Doesn’t Mean “Moderate” Understanding the Acute Problem Riddle in MDM. Let’s be honest — it makes sense to assume that if a patient

In American corporate culture, the final week of the year often serves as a time for reflection and big-picture thinking. At Chirok, we take this opportunity to review all our decisions through the lens of our core value: improving revenue cycle performance according to each client’s unique definition of success.
Whether you’re a small practice or a large healthcare organization, Chirok Health is here to help you achieve precision, efficiency, and success. Start the conversation for a tailored solution.
© 2025 Chirok Health. All rights reserved.