How Under-Utilized Counseling Codes Left $129,613 on the Table Despite Supporting Documentation
Why Under-Utilized Counseling Codes Are a Hidden Revenue Risk for Healthcare Leaders
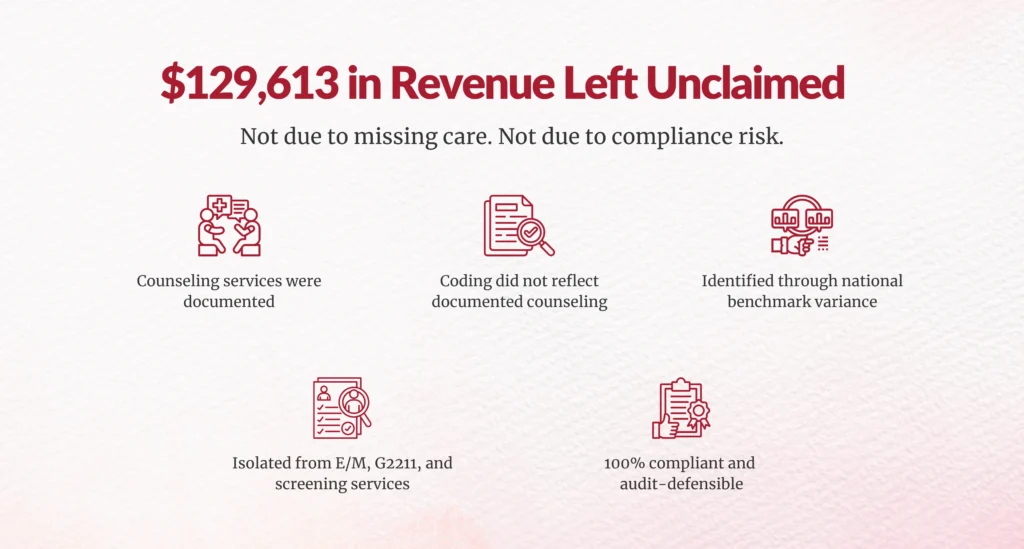
Healthcare leaders rarely worry about counseling codes being a major revenue lever. Yet, in one recent benchmark-driven coding analysis, $129,613 in legitimate, compliant reimbursement was left uncollected, not because care wasn’t delivered, not because documentation was missing, and not because of compliance risk, but because counseling services were under-utilized at the coding level.
If you oversee CDI, HIM, or revenue cycle performance, this is a scenario you should pay close attention to, because it’s far more common than most organizations realize.
What Actually Caused the $129,613 Revenue Loss?
The short answer: missed code capture, not missed care.
A national benchmark comparison identified $129,613 in potential incremental reimbursement tied specifically to counseling services. This amount was isolated from other opportunities, such as E/M leveling, screening services, or CMS add-on codes like G2211, making it a clean, defensible revenue leakage number attributable to counseling codes alone.
Importantly, this opportunity was identified despite supporting clinical documentation already being present. Providers documented counseling time, risk discussions, care planning, and patient education, but those services were not consistently translated into billable counseling codes.
This is the kind of revenue loss that hides in plain sight.
Why Is Under-Utilization of Counseling Codes So Common?
Because counseling services sit at the intersection of clinical nuance, documentation standards, and coding interpretation, that intersection is where breakdowns often occur.
National benchmarking by specialty showed a clear variance between:
- Expected counseling utilization rates, and
- Actual coded counseling frequency
This variance signals systemic under-coding, not isolated errors.
According to the American Medical Association (AMA), counseling and coordination of care can be used to support code selection when time-based criteria are met, yet many organizations default to conservative coding due to fear of audits or unclear internal guidance
The result? Counseling is delivered, documented, and clinically necessary, but financially invisible.
Was This a Compliance or Audit Risk Issue?
No, and that distinction matters.
The benchmark analysis explicitly states that the findings do not imply inappropriate billing. Instead, the opportunity reflects the missed capture of compliant services.
Every identified counseling opportunity was:
- Contingent on compliant documentation
- Aligned with CMS and AMA guidance
- Subject to payer-specific rules
- Audit-defensible
CMS has long clarified that when counseling or coordination of care dominates a visit and documentation supports time thresholds, it can be used for code selection
In other words, this $129,613 gap represents legitimate reimbursement, not aggressive optimization or risk exposure.
If Documentation Was Present, Where Did the Process Break Down?
This is the core operational insight leaders should focus on.
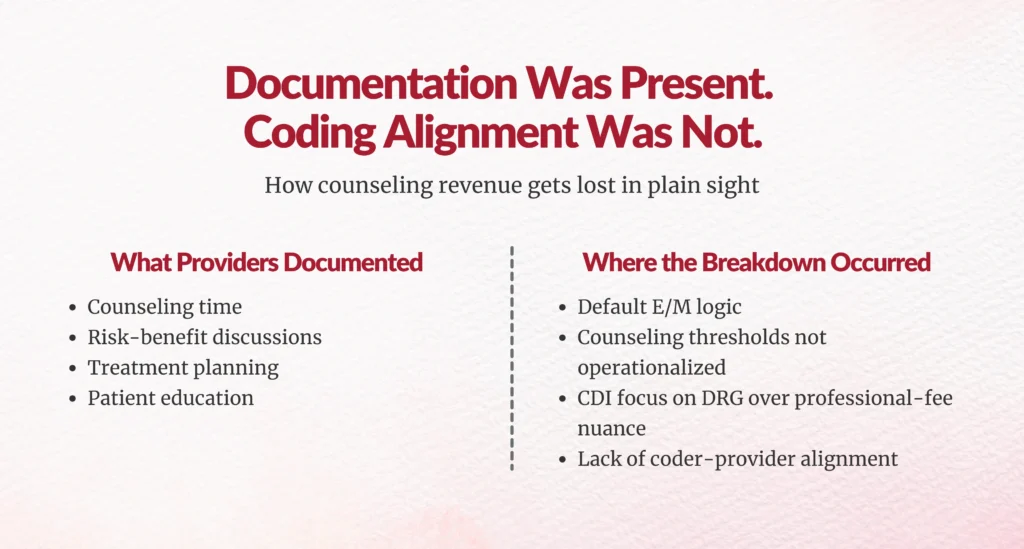
The problem wasn’t documentation quality; it was documentation translation
Providers documented:
- Counseling time
- Risk-benefit discussions
- Treatment planning
- Patient education
But the coding workflow failed to recognize, validate, and apply counseling rules consistently.
This gap typically occurs when:
- Coders default to problem-based E/M logic
- CDI programs prioritize DRG or diagnosis capture over professional-fee nuances
- Counseling thresholds aren’t operationalized in coder education
- Providers aren’t coached on documenting time in a codable format
AHIMA has repeatedly highlighted that documentation alone does not ensure accurate reimbursement; coding interpretation and alignment are equally critical.
Why Should CFOs and Revenue Leaders Care About “Only” $129,613?
Because this number scales, fast.
This $129,613:
- Came from one discrete service category
- Was identified through benchmark variance, not exhaustive auditing
- Did not require new services, new providers, or new contracts
Now ask yourself:
- What happens if similar under-utilization exists across other specialties?
- What if counseling under-coding is compounded by missed G2211, prolonged services, or care management codes?
- What does this look like over 12–24 months?
HFMA estimates that revenue leakage from coding misalignment and under-capture can range from 1–3% of net patient revenue, often without triggering denials
That makes counseling codes a high-confidence, low-risk recovery area.
Why Is Benchmarking Critical to Identifying This Type of Loss?
Because internal reviews rarely catch what feels “normal.”
Benchmarking works because it answers one essential question:
Are we coding the same way our peers are—when documentation supports it?
In this case, national specialty-level benchmarks revealed a consistent gap between:
- Expected counseling utilization, and
- Actual billing patterns
This confirmed the loss was systemic, reproducible, and data-driven, not anecdotal.
Without external benchmarks, under-utilization quietly becomes institutional behavior.
What Should CDI, HIM, and RCM Leaders Do Differently?
1. Treat counseling codes as a revenue integrity issue, not a coding footnote
Counseling under-capture is not a productivity problem, it’s a revenue integrity blind spot.
2. Operationalize counseling thresholds
Ensure coders and CDI teams are aligned on:
- Time-based criteria
- Documentation requirements
- Specialty-specific expectations
3. Use benchmark variance as an early warning system
Don’t wait for denials or audits. Benchmarking surfaces missed revenue before compliance risk appears.
4. Align CDI and professional-fee coding strategies
Most CDI programs focus on inpatient or diagnosis-driven outcomes. Counseling capture requires intentional professional-fee alignment.

What’s the Bigger Takeaway for Healthcare Leaders?
The $129,613 loss wasn’t dramatic. It wasn’t obvious. And it didn’t trigger alarms.
That’s exactly why it matters.
Counseling codes represent a quiet, compliant, repeatable revenue opportunity that many organizations overlook, not because they’re doing anything wrong, but because no one is looking closely enough.
If you’re responsible for:
- Documentation integrity
- Coding accuracy
- Revenue predictability
- Financial sustainability
Then under-utilized counseling codes aren’t a small issue. They’re a signal.
And signals are what smart leaders act on, before they become patterns.
FAQs
1. What does it mean when counseling codes are “under-utilized”?
Under-utilized counseling codes mean that counseling services were clinically delivered and documented, but not fully captured in billing. This typically happens when counseling time, care coordination, or patient education meets coding criteria but is not translated into the appropriate billable counseling or time-based codes.
2. How can revenue be lost if documentation already supports counseling services?
Revenue is lost when documentation exists but coding workflows fail to recognize or apply counseling rules. Providers may document counseling time and decision-making, but if coders default to problem-based E/M logic or lack clear guidance on counseling thresholds, those services remain financially invisible.
3. Is capturing counseling codes a compliance or audit risk?
No, when done correctly. Counseling codes are CMS- and AMA-aligned, and when documentation supports time-based criteria, they are fully compliant and audit-defensible. The $129,613 identified in the analysis represented legitimate reimbursement, not aggressive or risky billing practices.
4. Why don’t internal audits usually catch missed counseling code opportunities?
Internal audits often focus on overcoding risk, denials, or DRG accuracy, not under-capture. Without external national benchmarking, under-utilization can appear “normal” internally, allowing revenue leakage to persist unnoticed.
5. Why should CFOs and revenue leaders care about counseling codes?
Because counseling under-capture scales across providers, specialties, and time. HFMA estimates that 1–3% of net patient revenue can be lost to coding misalignment. Counseling codes represent a low-risk, high-confidence revenue integrity opportunity that does not require additional services or staffing.
6. What is the first step to fixing under-utilized counseling codes?
The first step is benchmarking counseling utilization against national specialty norms. This identifies where your organization deviates from peers and pinpoints missed revenue that is already supported by documentation, allowing CDI, HIM, and RCM teams to correct workflows without increasing compliance risk.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.





