5 Signs Your CDI Program Needs Improvement and When to Seek External Support
How Do You Know When Your CDI Program Is No Longer Delivering Results?
Your CDI program needs improvement when it no longer moves core outcome metrics CMI, denials, audit risk, provider engagement, and financial integrity, despite ongoing effort. When those gaps persist or widen, external CDI support becomes a strategic necessity, not a last resort.
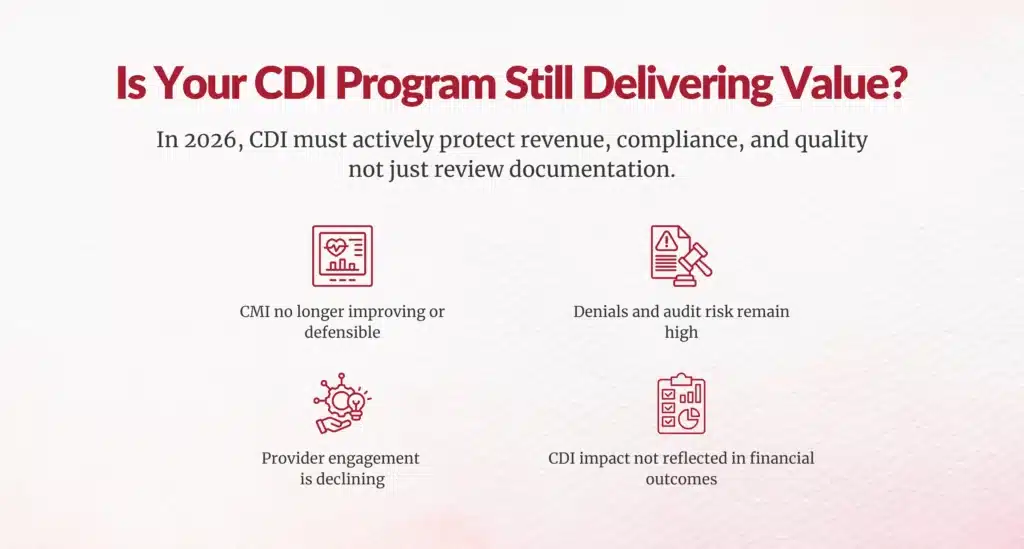
In 2026, CDI is no longer a “documentation improvement” function alone. It is a risk mitigation, reimbursement protection, and quality strategy. Programs that fail to evolve are now exposing organizations to revenue leakage, compliance risk, and value-based performance penalties.
Below, CDI leaders and industry benchmarks consistently point to five warning signs that indicate when internal programs are falling short and when it’s time to bring in outside expertise.
Why Is Declining or Stagnant Case Mix Index (CMI) a Red Flag for CDI Programs?
Sign 1: Declining or Stagnant Case Mix Index (CMI)
A mature CDI program should demonstrate sustained, defensible CMI improvement over time, not volatility or flat performance.
More importantly, as clinician education improves, the gap between pre-query and post-query CMI should narrow, signaling better frontline documentation rather than reactive querying.
When CMI stagnates or declines despite active CDI efforts, it typically indicates one or more of the following:
- Documentation quality is not improving at the source
- Queries lack clinical depth or validation strength
- Provider engagement is weak or inconsistent
- CDI reviews are retrospective rather than concurrent
This is not just a CDI issue; it’s a direct reimbursement and compliance issue. CMS and commercial payers increasingly scrutinize CMI spikes without supporting documentation patterns, making stagnant or erratic CMI a warning sign worth immediate attention.
Why it matters in 2026:
With increasing audit focus on DRG integrity and medical necessity, “defensible CMI” matters more than higher CMI.
How Do Rising Denials and Audit Risk Signal CDI Failure?
Sign 2: Persistent Rising Denial Rates and Audit Vulnerability
An effective CDI program should reduce denials, not coexist with them.
If your organization continues to experience:
- Medical necessity denials
- Insufficient documentation denials
- DRG downgrades post-payment
- Fear payer audits
- Rely on aggressive or poorly structured queries
- Face compliance or whistleblower concerns
At that point, CDI may be increasing risk rather than reducing it.
What Does Low Provider Query Response Really Say About Your CDI Program?
Sign 3: Exceptionally High Query Abandonment and Low Provider Response Rates
One of the clearest operational signals of CDI distress is low provider query engagement.
Industry studies show that up to 60% of CDI queries go unanswered in many organizations, representing lost revenue, lost quality scores, and lost credibility.
Low response rates usually stem from:
- Excessive workflow friction
- Poor perception of CDI value
- Low-quality or marginal queries
- Lack of integration into clinical workflows
- Absence of accountability
High-performing programs share a critical differentiator:
87.5% have formal query escalation and accountability policies in place.
Without leadership-backed accountability, non-response becomes normalized and CDI loses influence fast.
Why Are Staffing Shortages and Skills Gaps Undermining CDI Performance?
Sign 4: Chronic Workforce Shortages, High Turnover, and Skills Gaps
CDI cannot succeed without stable, skilled resources.
Warning signs include:
- Persistent vacancies or reliance on overtime
- High turnover eroding institutional knowledge
- Burnout from unrealistic workloads
- Inability to recruit certified CDI professionals
The CDI workforce shortage is well-documented. The U.S. Bureau of Labor Statistics projects continued growth in health information roles, but the supply of experienced CDI specialists is not keeping pace.
Equally damaging are skills gaps, particularly in:
- HCC / RAF capture
- Clinical validation
- ICD-10 specificity
- High-acuity specialties (cardiology, orthopedics, behavioral health)
When CDI expertise doesn’t match your case complexity, performance ceilings become unavoidable.
What Happens When CDI Lacks Governance, Metrics, and Executive Alignment?
Sign 5: Absence of Governance, Clear Metrics, and Stakeholder Alignment
The most dangerous CDI problem is structural invisibility.
Common indicators include:
- No clearly defined CDI mission
- Weak executive sponsorship
- Activity metrics replacing outcome metrics
- Silos between CDI, HIM, coding, and clinicians
- CDI excluded from EHR, quality, or value-based initiatives
CFOs should be especially cautious of vanity metrics high query counts or CMI gains that don’t correlate with:
- Denial reduction
- Audit outcomes
- Net revenue integrity
Without governance and alignment, CDI becomes busy but not effective.
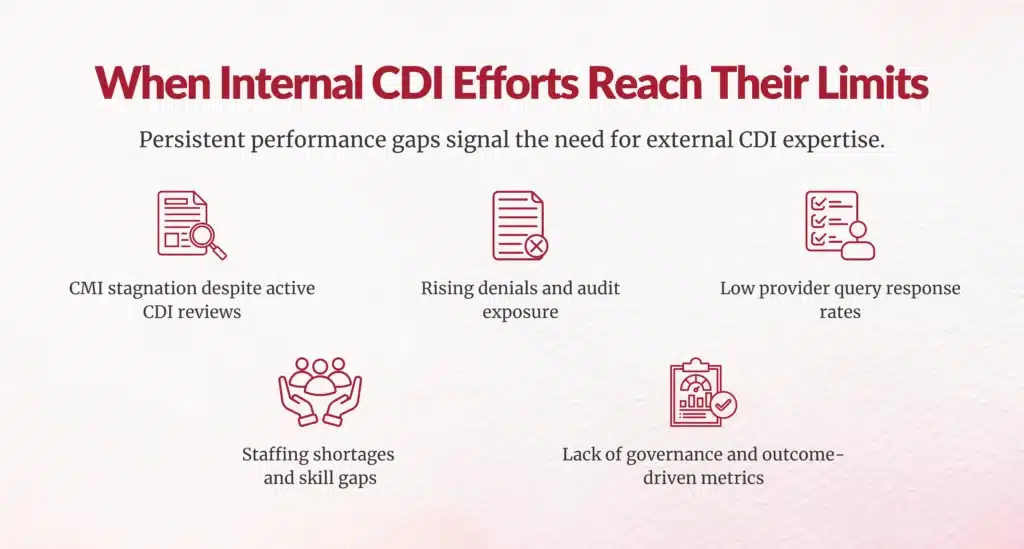
When Should Healthcare Organizations Seek External CDI Support?
External CDI support is most effective when used strategically, not reactively.
You should strongly consider outside expertise when:
1. Internal Capability Gaps Exist
Your team lacks deep expertise in HCC/RAF, clinical validation, or specialty-specific documentation.
2. Workforce Pressures Are Unsustainable
Staffing shortages or burnout prevent progress despite leadership awareness.
3. You Need an Objective Program Assessment
External reviewers identify blind spots internal teams may miss due to proximity or politics.
4. Program Redesign Is Required
Your CDI structure no longer aligns with fee-for-service, value-based care, or payer scrutiny.
5. Audit or Compliance Risk Is Escalating
Specialized expertise is needed to withstand payer, CMS, or RADV audits.
6. Time-Bound Initiatives Demand Focus
ICD-10 updates, EHR transitions, or enterprise CDI audits require short-term intensity.


What Should CDI Leaders Prioritize for 2026?
As CDI evolves in 2026, high-performing organizations are focusing on:
- Concurrent, clinically integrated CDI models
- Risk-adjustment and quality alignment
- Provider-facing education, not just querying
- Hybrid internal–external CDI staffing models
- Audit defensibility over short-term revenue gains
The most mature programs recognize that external CDI support is not a failure signal it’s a maturity signal.
Final Takeaway for CDI, HIM, and Revenue Cycle Leaders
If your CDI program is not improving CMI sustainably, reducing denials, engaging providers, stabilizing staffing, and protecting audit readiness, doing more of the same will not fix it.
Strategic external CDI support brings:
- Specialized expertise
- Scalable capacity
- Faster improvement cycles
- Stronger credibility with clinicians and executives
In 2026, the question is no longer “Can we manage CDI internally?”
It’s “Are we willing to invest in the expertise required to do CDI right?”
FAQs
What are key signs that a CDI program is no longer delivering measurable results?
Key signs include stagnant/declining CMI, persistent rising denial rates, high query abandonment (>60%), chronic staffing shortages/high turnover, and lack of governance, metrics, or executive alignment.
How does a stagnant or declining Case Mix Index (CMI) signal CDI program issues?
Stagnant CMI shows reliance on reactive queries instead of frontline clinician education, poor documentation patterns, and vulnerability to CMS scrutiny on DRG integrity and medical necessity.
Why do persistent rising denial rates indicate CDI program failure?
Rising denials mean CDI fails to produce payer-proof documentation; 80% of CMS improper payments stem from documentation/medical necessity gaps that CDI should prevent.
What does a high query abandonment rate mean for CDI effectiveness?
High abandonment (>60%) signals workflow friction, low provider value perception, marginal queries, and absent accountability; top programs enforce escalation policies.
How do staffing shortages and skills gaps undermine a CDI program?
Shortages create performance ceilings, high turnover disrupts continuity, and gaps in HCC/RAF/clinical validation expertise fail complex cases amid industry-wide shortages.
Why is governance, clear metrics, and executive alignment critical for CDI success?
Prevents vanity metrics like query volume; ties CDI to financials, denials, audits; ensures stakeholder buy-in across HIM, RCM, finance for sustained impact.
When should a healthcare organization consider external CDI support?
When facing capability gaps (HCC/specialty), unsustainable workforce pressures, need objective audits, program redesign, escalating audit risk, or time-bound initiatives.
How can external CDI support improve documentation integrity and financial outcomes?
Delivers specialized expertise, uncovers internal blind spots, redesigns workflows, reduces denials, achieves defensible CMI gains, and recovers revenue.
What performance measures should CDI leaders track to assess program health?
Track CMI trends/gaps, denial overturn rates, query response/agreement rates, DRG shifts, audit outcomes, and net financial impact via executive dashboards.
How does a mature CDI program evolve with concurrent review and integrated workflows?
Concurrent review enables real-time engagement/gap fixes during care (70–80% inpatient penetration), integrates FFS/value-based care for proactive documentation.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.