How to Choose Expert Scalable Retrospective Reviews Support for Payors?
How do you choose expert, scalable retrospective review support without increasing organizational risk?
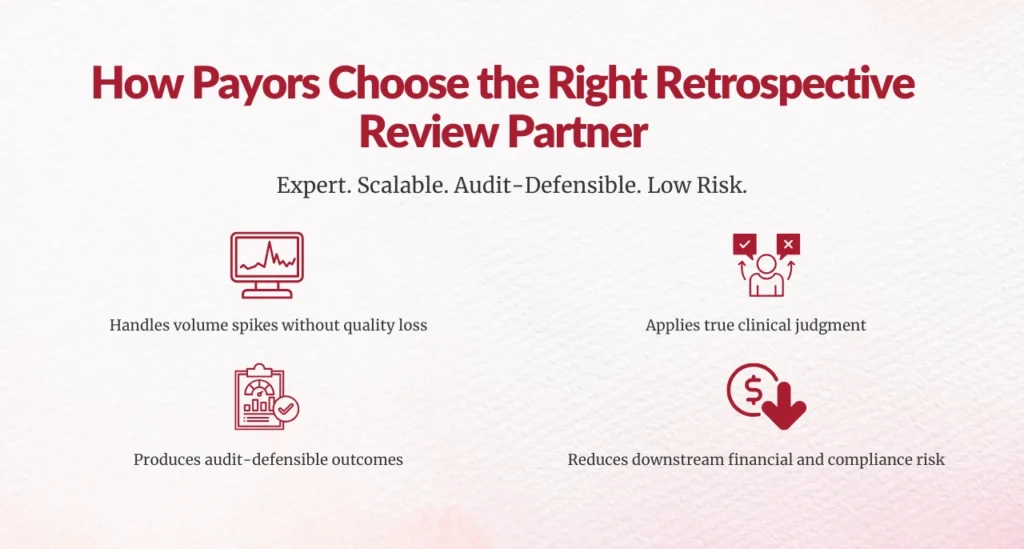
Choosing expert, scalable retrospective review support comes down to this:
You need a partner that can handle volume spikes, apply real clinical judgment, and produce audit-defensible outcomes, without creating downstream risk for your organization.
That’s what leaders like you are ultimately searching for.
Now let’s walk through how you evaluate that support the right way.
Why is retrospective review support more critical for payors today than ever before?
You already know retrospective reviews matter. What’s changed is how much they matter—and what’s at stake when they go wrong.
Payors are facing:
- Increased RADV and post-payment audits
- Heightened scrutiny around risk adjustment accuracy
- Persistent workforce shortages
- Tighter regulatory enforcement
According to the Centers for Medicare & Medicaid Services (CMS), improper payments across Medicare programs totaled $31.2 billion in FY 2023, with documentation and coding issues cited as leading contributors.
For you, that translates into:
- Revenue leakage
- Audit exposure
- Compliance risk
- Executive accountability
Retrospective reviews are no longer a back-office function, they are a risk mitigation strategy.
What does “expert” retrospective review support actually mean?
This is where many organizations struggle, because “expert” is one of the most misused words in this space.
Expert retrospective review support goes beyond:
- Code validation
- Checklist-based audits
- High-volume chart processing
True expertise includes:
- Clinical validation grounded in patient acuity
- Interpretation of CMS, payer, and regulatory guidance
- Ability to explain why a diagnosis is supported, or not
The American Health Information Management Association (AHIMA) emphasizes that retrospective reviews must focus on clinical documentation integrity and defensibility, not just technical coding accuracy.
If a vendor cannot clearly articulate clinical rationale in a way that stands up to audit, they are not providing expert support, no matter how fast they work.
Why clinical validation matters more than coding accuracy alone?
Coding accuracy tells you what was reported.
Clinical validation tells you whether it was true.
From a payor perspective, clinical validation is what:
- Reduces appeal volumes
- Protects RAF integrity
- Strengthens audit defense
Without it, retrospective reviews become a numbers exercise instead of a risk-control mechanism.
How do you evaluate scalability without sacrificing quality?
This is one of the most important, and most misunderstood, questions leaders ask.
Scalability is not about adding more reviewers quickly. It’s about maintaining:
- Consistent interpretation of guidelines
- Inter-rater reliability (IRR)
- Turnaround times under pressure
According to HFMA, 67% of healthcare organizations report staffing shortages impacting audit and review workflows, leading to delays and accuracy issues.
You should be asking:
- How does the partner maintain quality when volume doubles?
- What governance model ensures consistency across reviewers?
- Is QA proactive or reactive?
If quality drops as volume rises, scalability becomes a liability.
What does sustainable scalability look like in practice?
Sustainable scalability includes:
- Pre-trained, credentialed reviewer pools
- Embedded quality assurance
- Standardized clinical decision frameworks
- Clear escalation pathways
If scaling depends on last-minute hiring or retraining, risk increases, not efficiency.
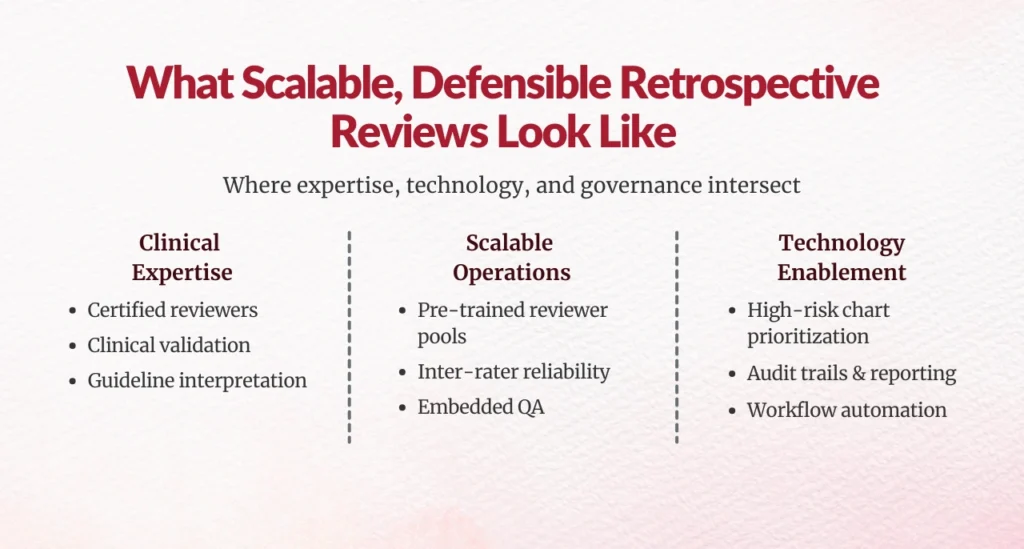
What role should technology play in retrospective reviews?
Technology should enable, not replace, clinical expertise.
Strong retrospective review programs use technology to:
- Prioritize high-risk charts
- Reduce manual chart navigation
- Track decisions and rationales
- Produce defensible audit trails
A Health Affairs study found that technology-enabled review programs reduced administrative costs by up to 30% while improving compliance outcomes.
For leaders like you, technology should answer one question clearly:
Does this make clinical reviewers more accurate and more consistent?
If the answer is no, it’s just overhead.
Why is audit and regulatory defensibility non-negotiable?
Because at the end of the day, you own the outcome.
CMS has consistently reinforced that unsupported diagnoses, especially in risk-adjusted models, will not be accepted.
That means every retrospective review decision must be:
- Clinically justified
- Clearly documented
- Defensible long after the review is complete
If a vendor cannot stand behind its findings during audits or appeals, the risk shifts directly to your organization.
What should defensible retrospective review documentation include?
At a minimum:
- Clear clinical rationale
- Alignment to official guidelines
- Transparent decision logic
- Complete audit trails
Anything less creates exposure.
How should you think about ROI from retrospective reviews?
This is where many programs fall short, not because ROI doesn’t exist, but because it’s poorly defined.
Effective retrospective review support delivers ROI through:
- Accurate identification of overpayments and underpayments
- Reduced audit fallout
- Improved RAF stability
- Lower internal staffing burden
McKinsey reports that organizations combining expert clinical review with analytics-driven workflows achieve 2–5% improvement in revenue integrity outcomes annually.
You should expect reporting that clearly shows:
- Financial impact
- Error trend reduction
- Audit success rates
If ROI can’t be explained in plain language, it won’t survive executive scrutiny.
Why does clinical alignment with providers matter for payors?
This is often overlooked, but it matters more than ever.
When retrospective reviews feel disconnected from real-world care:
- Appeals increase
- Provider trust erodes
- Improvement stalls
Expert support ensures reviews reflect true patient acuity, not theoretical documentation standards. That alignment reduces friction and improves long-term documentation quality.
What questions should you ask before selecting a retrospective review partner?
Before making a decision, ask:
- Who performs the reviews, and what are their credentials?
- How do you ensure consistency across reviewers?
- How do you stay aligned with evolving CMS guidance?
- What quality and governance models are in place?
- How do insights feed back into CDI improvement?
Strong partners answer these directly. Weak ones avoid specifics.


How can you move forward with confidence as a leader?
Choosing expert, scalable retrospective reviews support is not about outsourcing work—it’s about protecting revenue, compliance, and leadership credibility.
The right partner:
- Scales with your organization
- Delivers defensible outcomes
- Reduces long-term risk
If retrospective reviews feel overwhelming, that’s not a failure; it’s a sign your organization needs a more mature approach.
Handled correctly, retrospective reviews become a strategic advantage, not a constant fire drill.
And that’s exactly where payor leaders need to be.
FAQs
1. What is retrospective review support for payors?
Retrospective review support helps payors evaluate medical records after services are rendered to confirm that diagnoses, procedures, and documentation are clinically supported, accurately coded, and audit-defensible. These reviews are critical for risk adjustment accuracy, payment integrity, and regulatory compliance.
2. Why do payors need expert retrospective review support instead of internal teams alone?
Audit volumes, regulatory complexity, and staffing shortages make it difficult for internal teams to scale without sacrificing accuracy. Expert retrospective review support provides specialized clinical validation expertise, scalable capacity, and structured quality governance while reducing operational strain.
3. How is expert retrospective review support different from basic chart audits?
Basic chart audits focus mainly on coding accuracy. Expert retrospective review support applies clinical judgment, interprets CMS and payer guidance, and clearly documents why a diagnosis is supported or not, making findings defensible during audits and appeals.
4. How do retrospective reviews help reduce audit and compliance risk?
Retrospective reviews identify unsupported or high-risk diagnoses before they become audit findings. When performed correctly, they produce clear clinical rationales, guideline alignment, and audit trails that reduce exposure during RADV audits, OIG reviews, and payer-driven audits.
5. What does scalable retrospective review support really mean for payors?
Scalability means maintaining accuracy, consistency, and turnaround times even as review volumes increase. True scalable support relies on pre-trained reviewer pools, embedded quality assurance, and strong governance, not rapid hiring that increases risk.
6. How can payors measure the ROI of retrospective review programs?
ROI is measured through both financial and operational outcomes, including dollars recovered or protected, reduced audit findings, improved RAF stability, lower appeal rates, and reduced internal staffing burden. Clear, executive-level reporting is essential to demonstrate value.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.





