15 Things to Expect From a Payor-Led Retrospective Review Engagement
Why Payor-Led Retrospective Reviews Are Now a Financial and Audit Imperative
If you are a payor leader in charge of Risk Adjustment or Provider Network Management, a payor-led retrospective review engagement is no longer a “nice-to-have.” It is a core financial, compliance, and performance strategy.
The short answer, for most payors, is not consistently.
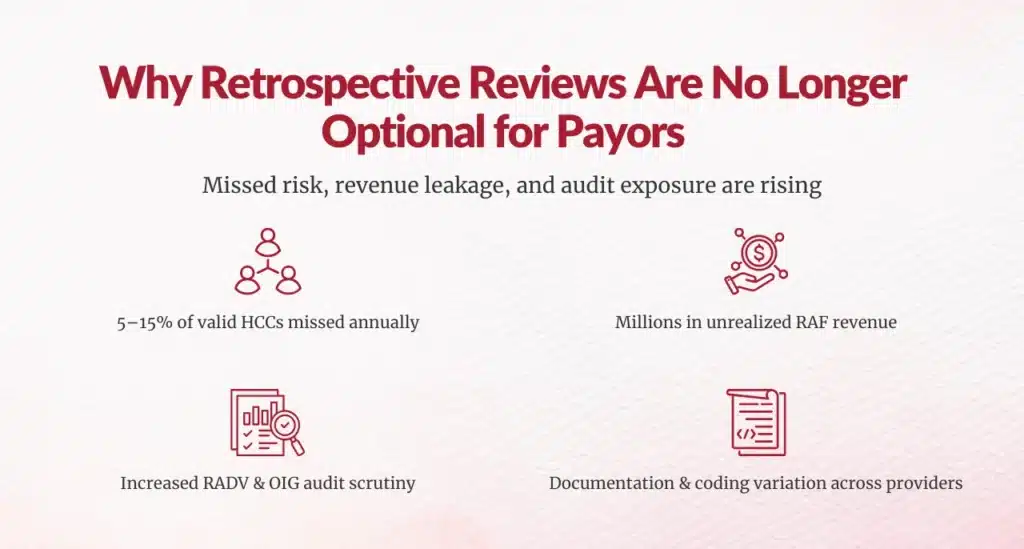
Industry research shows that 5–15% of valid HCCs are often missed due to documentation gaps, coding variation, or workflow limitations, translating into millions of dollars in unrealized revenue and elevated RADV exposure for Medicare Advantage and value-based populations.
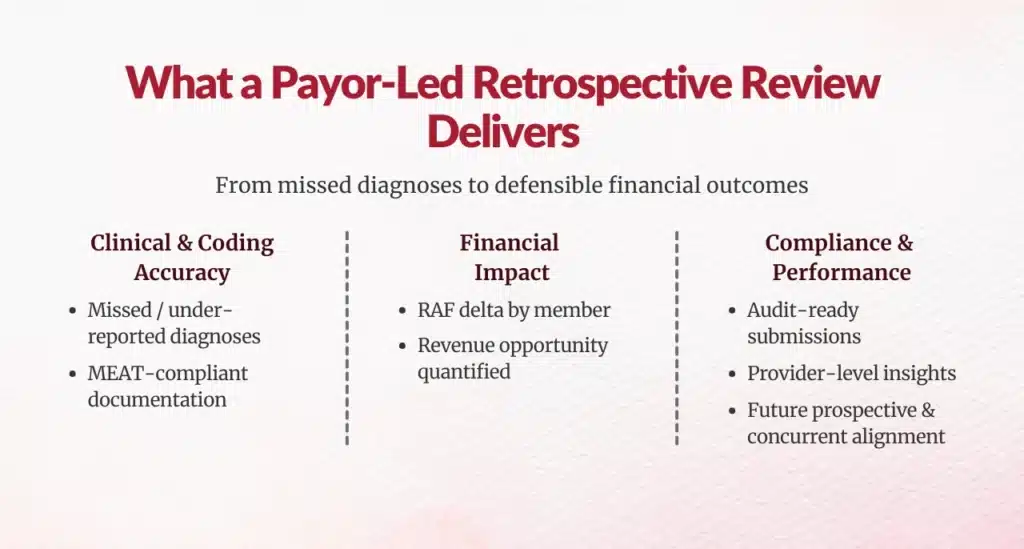
What Should You Expect From a Payor-Led Retrospective Review, at a High Level?
- Identify missed, under-reported, or insufficiently documented diagnoses
- Quantify RAF impact and financial opportunity
- Strengthen payment integrity and audit readiness
- Surface provider-level documentation and coding trends
- Feed insights into future prospective and concurrent strategies
How Exactly Does Concurrent Coding Increase E/M Volume?
1. Clear Alignment on Why the Review Is Being Conducted
- RAF optimization
- CMS audit defense
- Payment accuracy
- Provider performance benchmarking
- Preparation for upcoming model changes
2. A Data-First, Analytics-Driven Review Scope
- Claims history
- Risk adjustment submissions
- Encounter data
- Member demographics
- Suspect condition analytics
Advanced programs use AI and NLP to identify likely missed HCCs across structured and unstructured data sources, improving scale and precision.
3. Prioritization of High-Impact Members and Conditions
- High-cost or high-utilization members
- Chronic and progressive conditions
- Historically under-captured HCC categories
- Providers with inconsistent documentation patterns
4. Use of Certified, Audit-Ready Coding Resources
- CRC, CPC, or CCS-certified coders
- Demonstrated Medicare Advantage and HCC expertise
- Strong understanding of CMS risk adjustment rules
5. Strict Application of MEAT Documentation Standards
Expect every identified diagnosis to meet MEAT criteria:
- Monitor
- Evaluate
- Assess
- Treat
If a condition does not meet MEAT, it should not be submitted, regardless of financial upside.
6. Transparent Quantification of RAF and Revenue Impact
- Net new HCCs identified
- RAF delta per member
- Aggregate RAF lift
- Estimated revenue impact
- Confidence intervals and assumptions
7. Clear Differentiation Between Recoverable and Non-Recoverable Findings
- Diagnoses eligible for submission
- Diagnoses requiring additional documentation
- Diagnoses excluded due to compliance risk
8. Provider-Level Documentation and Coding Insights
- Providers with consistent documentation gaps
- Specialty-specific risk capture trends
- Education opportunities by condition category
9. Defined Governance and Oversight Structure
- Coding QA audits
- Clinical validation layers
- Compliance sign-off
- Version-controlled documentation trails
10. RADV and OIG Audit Alignment
Given CMS’s intensified RADV enforcement, you should expect the retrospective methodology to mirror audit standards, not internal convenience.
CMS has estimated improper MA payments in the billions annually, making defensibility non-negotiable.
11. Integration With Prospective and Concurrent Programs
- Prospective suspecting models
- Concurrent documentation improvement workflows
- Provider education initiatives
12. Clear Compliance Risk Assessment
- Identification of compliance vulnerabilities
- Documentation of excluded diagnoses
- Risk mitigation recommendations
13. Provider Communication and Change Management Planning
- How and when providers are informed
- Educational content tailored to documentation gaps
- Non-punitive improvement frameworks
14. Realistic ROI and Performance Expectations
15. A Scalable, Repeatable Operating Model
- A recurring capability
- A learning system
- A continuously improving function







Best Practices for Payor Leaders to Maximize Retrospective Review Value
Start With Analytics, Not Charts
Use data science to guide effort — not manual sampling.
Build Audit Readiness Into Every Step
If it cannot survive RADV, it should not be submitted.
Close the Loop With Providers
Turn findings into forward-looking documentation improvement.
Measure Trends, Not Just One-Year Gains
Sustained improvement matters more than short-term lift.
Final Takeaway for Risk Adjustment and Network Leaders
When designed strategically, these engagements:
- Improve RAF accuracy
- Reduce audit exposure
- Strengthen provider documentation
- Support long-term value-based success
As a leader, your role is to ensure the engagement is data-driven, audit-defensible, provider-aware, and strategically integrated.
When those elements are in place, retrospective reviews become one of the most powerful tools in your risk adjustment arsenal.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.





