25 Ways How Concurrent Coding Improves RAF Scores Without Triggering Upcoding Risk
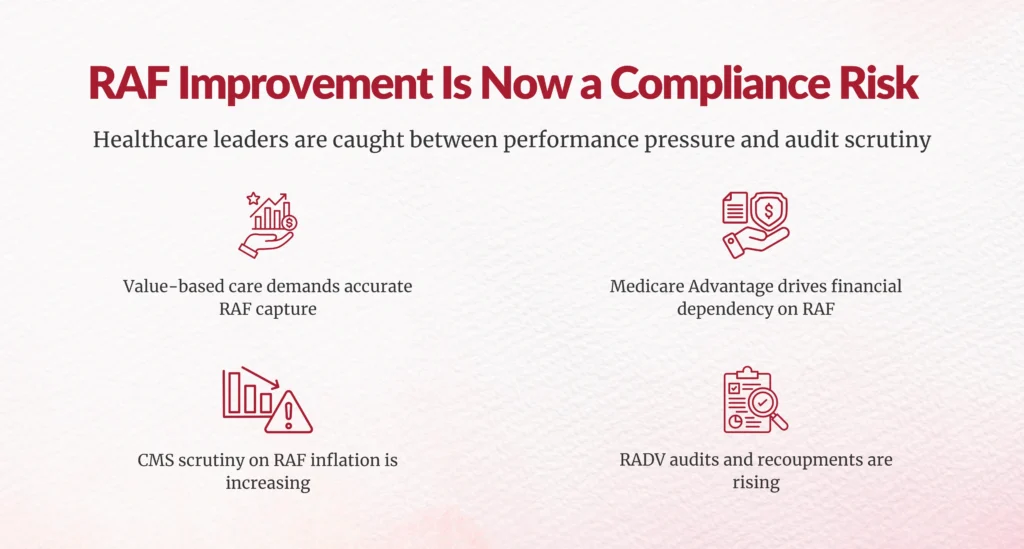
Why RAF Improvement Has Become a High-Risk Leadership Challenge?
If you’re accountable for RAF performance, you’re under pressure from two sides. On one side, value-based contracts, Medicare Advantage plans, and payors expect accurate risk capture. On the other, CMS scrutiny around RAF inflation, RADV audits, and upcoding allegations has never been higher.
This creates a real leadership challenge: How do you improve RAF scores without increasing compliance risk?
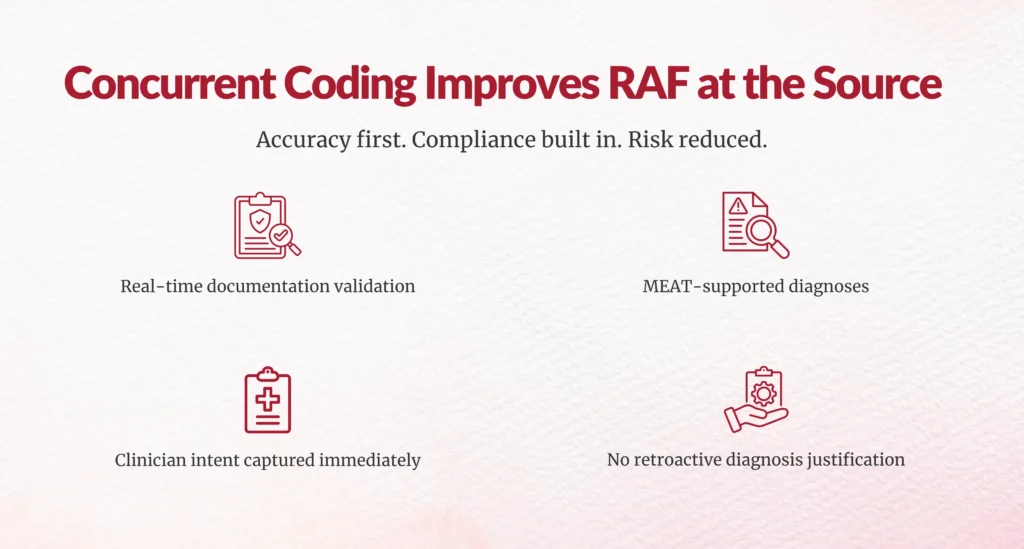
The most sustainable answer isn’t retrospective coding or aggressive querying. It’s concurrent coding, a model where coding and CDI review happen during or immediately after the patient encounter. When implemented correctly, concurrent coding improves RAF scores by improving documentation accuracy at the source, not by retrofitting diagnoses later.
Below are 25 specific, operational ways concurrent coding improves RAF scores without triggering upcoding risk, explained clearly and practically so you can evaluate and apply them across your organization.
Why Is Concurrent Coding a Safer Path to RAF Improvement?
RAF models reward accurate clinical documentation of patient complexity, not assumptions, not extrapolations, and not retrospective justification. Concurrent coding works because it captures clinical truth in real time, when documentation is most accurate and defensible.
How Does Concurrent Coding Improve RAF Scores Without Increasing Compliance Exposure?
1. Real-time diagnosis capture prevents missed HCC conditions
Concurrent coding ensures that chronic and complex conditions addressed during care are documented before the encounter closes. Many RAF losses occur simply because a condition was clinically managed but never explicitly documented. Real-time review closes that gap.
2. MEAT-supported documentation is reinforced at the point of care
Concurrent coding validates that diagnoses meet MEAT criteria, Monitored, Evaluated, Assessed, or Treated, during the encounter itself. This makes RAF-impacting conditions defensible and aligned with CMS expectations.
3. Diagnostic specificity improves without exaggeration
Vague diagnoses like “diabetes” or “heart failure” are clarified in real time. This improves RAF accuracy while avoiding unsupported severity escalation that could trigger audits.
4. Provider clinical intent is captured while memory is fresh
Documentation completed close to care delivery reflects actual decision-making. This is far more credible than notes revised weeks later, which auditors often view with skepticism.
5. Annual RAF recapture gaps are reduced
Concurrent coding supports consistent documentation of chronic conditions each year, preventing missed recapture that lowers RAF performance in Medicare Advantage and value-based contracts.
6. CDI-provider collaboration becomes part of normal care delivery
Instead of disruptive retrospective queries, CDI support is integrated into daily workflows. This improves provider trust, engagement, and long-term documentation quality.
7. Physician query turnaround time drops dramatically
When clarification happens during the encounter, response times shrink from weeks to hours. This prevents incomplete documentation from flowing downstream.
8. Provider documentation habits improve over time
Repeated real-time feedback helps clinicians internalize documentation best practices. Over time, documentation improves naturally, without adding administrative burden.
9. Chronic condition visibility improves across encounters
Conditions like CKD, COPD, CHF, and diabetes complications are more consistently documented when addressed during care rather than inferred later.
10. Financial integrity stays aligned with clinical reality
Concurrent coding ensures RAF improvement is driven by clinical evidence, not revenue pressure. This alignment protects organizational credibility with payors and regulators.
11. AI-assisted tools surface gaps without auto-coding
AI highlights potential RAF-impacting conditions while human coders retain judgment. This preserves ethical oversight and reduces algorithm-driven risk inflation.
12. NLP uncovers documented risk hidden in clinical notes
Natural language processing identifies complexity already documented by providers but not yet codified, improving RAF completeness responsibly.
13. Retrospective interpretation errors are minimized
Concurrent coding eliminates guesswork by validating diagnoses directly with providers, reducing subjective interpretation that auditors challenge.
14. HCC documentation is grounded in clinical context
Diagnoses documented during care are supported by treatment decisions, labs, and assessments, making them far more defensible than retrospective additions.
15. High-impact RAF encounters receive priority
Concurrent workflows allow organizations to focus resources on encounters with the highest complexity and RAF impact instead of blanket retrospective reviews.
16. Chart rework and post-visit corrections decline
Immediate clarification reduces the need for documentation revisions, improving efficiency and lowering compliance noise.
17. Claims move faster through the revenue cycle
Cleaner documentation at the outset reduces delays, rejections, and downstream corrections, supporting both RAF accuracy and cash flow.
18. Administrative burden on HIM and RCM teams decreases
Fewer retrospective queries mean fewer follow-ups, fewer appeals, and less internal escalation.
19. First-pass coding accuracy improves significantly
Organizations using concurrent coding report first-pass accuracy rates approaching 80–90%, reducing downstream adjustments that attract audit attention.
20. Coder productivity increases without quality loss
Coders spend less time deciphering incomplete records and more time validating high-complexity cases, improving both output and consistency.
21. Audit defensibility improves through contemporaneous documentation
Documentation created at the time of care is more credible during RADV and OIG audits than retrospective updates.
22. Upcoding risk is reduced through real-time validation
Concurrent coding confirms documented conditions instead of inflating severity after the fact, keeping RAF growth grounded in clinical truth.
23. Longitudinal patient risk profiles become cleaner
Consistent real-time documentation improves population health analytics and performance tracking under value-based arrangements.
24. CMS scrutiny is addressed proactively
With increased oversight on RAF practices, concurrent documentation aligns organizations with regulatory expectations.
25. RAF strategies are future-proofed
As AI-driven audits expand, organizations with real-time, clinically grounded documentation will outperform retrospective correction models.
Real-World Impact: What Concurrent Coding Looks Like in Practice
To understand how concurrent coding improves RAF scores without increasing compliance risk, it helps to look at what happens when the model is applied consistently over time.
In one Medicare Advantage population, concurrent coding was introduced by Chirok Health in 2023 as part of a broader documentation accuracy initiative. Rather than relying on retrospective chart reviews, coding and CDI validation occurred during or immediately after patient encounters.
Instead of focusing on absolute RAF scores, what matters more is the year-over-year improvement trend:
- 2023 to 2024: RAF capture increased by approximately 1.8%
- 2024 to 2025: RAF capture increased by approximately 1.7%
- Sustained improvement over three years without documentation inflation
What’s notable here isn’t just the improvement itself, it’s how the improvement was achieved. There was no increase in aggressive querying, no retrospective diagnosis justification, and no spike in audit risk indicators.
The gains came from:
- More complete capture of already-managed chronic conditions
- Improved diagnostic specificity at the point of care
- Consistent MEAT-supported documentation
- Faster real-time clarification with providers
This is what compliant RAF improvement looks like in practice: steady, defensible growth driven by documentation accuracy, not coding pressure.

What Is the Bottom Line for Healthcare Leaders?
If your RAF strategy still relies heavily on retrospective chart reviews, you’re absorbing unnecessary risk. Concurrent coding improves RAF scores by fixing documentation at the source, not by correcting it later.
For CDI, HIM, RCM leaders, and CFOs, the takeaway is simple:
Accurate documentation today is the strongest audit defense tomorrow.
Concurrent coding is no longer just an operational enhancement. It’s a risk governance strategy for healthcare organizations navigating tighter regulation and growing financial scrutiny.
FAQs
1. What is concurrent coding, and how is it different from retrospective coding?
Concurrent coding is the practice of reviewing clinical documentation and assigning codes during or immediately after the patient encounter. Unlike retrospective coding—which relies on completed charts days or weeks later, concurrent coding captures diagnoses while clinical context is fresh, reducing missed HCCs, interpretation errors, and documentation gaps that negatively impact RAF scores.
2. How does concurrent coding improve RAF scores without leading to upcoding?
Concurrent coding improves RAF scores by ensuring diagnoses are documented accurately, specifically, and with proper clinical support at the point of care. Because conditions are validated in real time based on provider intent and treatment, RAF improvement comes from better accuracy, not inflated severity or retrospective justification,significantly reducing upcoding risk.
3. Does concurrent coding increase the burden on physicians?
When implemented correctly, concurrent coding actually reduces physician burden. Real-time clarification replaces delayed retrospective queries, minimizing follow-up messages, chart revisions, and end-of-year documentation pressure. Over time, providers also improve documentation habits organically through consistent, contextual feedback.
4. How does concurrent coding support audit readiness and RADV defense?
Documentation created during the encounter is more credible and defensible than post-hoc updates. Concurrent coding ensures RAF-impacting diagnoses meet MEAT criteria and are supported by clinical actions, strengthening audit trails and reducing exposure during RADV, OIG, and payor audits.
5. What role does technology play in concurrent coding for RAF accuracy?
Technology, such as AI-assisted coding tools and natural language processing (NLP), helps surface potential documentation gaps and risk indicators in real time. However, human oversight remains critical. The most effective concurrent coding programs use technology to augment, not replace, clinical judgment and coder expertise.
6. Which healthcare organizations benefit most from concurrent coding?
Concurrent coding is especially valuable for organizations participating in Medicare Advantage, value-based care models, and risk-adjusted contracts. Hospitals, health systems, physician groups, and MSOs with high chronic disease populations see the greatest RAF and compliance benefits due to improved documentation consistency and reduced retrospective risk.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.