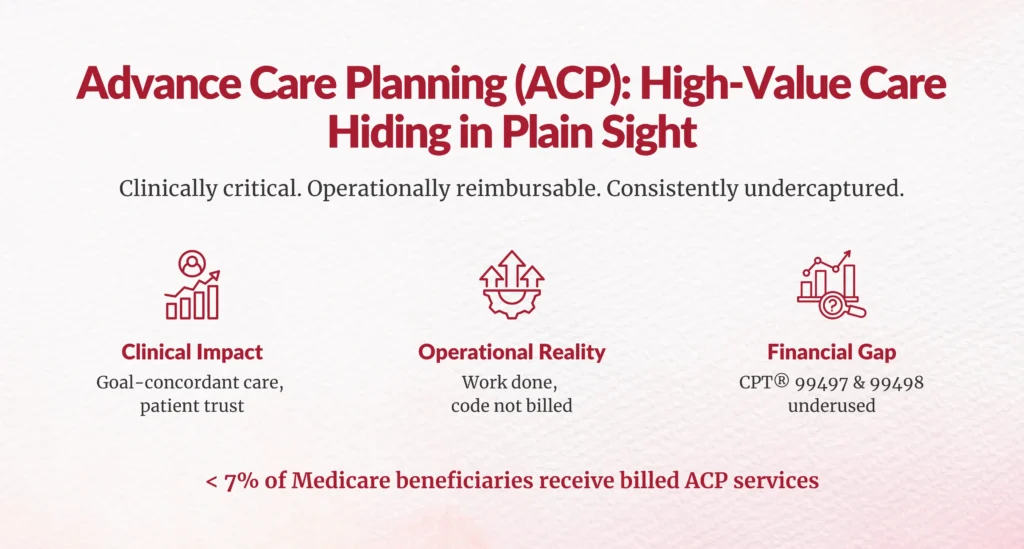
Advance Care Planning (ACP): An Underused Service for Medicare Beneficiaries That Matters, Clinically and Operationally
Advance Care Planning (ACP) is one of the clearest examples of high-value clinical work that consistently goes undercaptured in Medicare billing. Despite being covered, reimbursable, and strongly aligned with quality and patient-centered care goals, CPT® codes 99497 and 99498 remain significantly underutilized across primary care and specialty settings.
If you oversee clinical documentation integrity (CDI), HIM, revenue cycle operations, or financial performance, this gap should concern you, not just from a revenue perspective, but from a care delivery and compliance standpoint.
The short answer to the core question is this:
Advance Care Planning is clinically essential, financially legitimate, and operationally achievable, but only when organizations treat it as a structured service instead of an informal conversation.
Let’s break down what that means for your organization.
What Is Advance Care Planning (ACP), and Why Does It Matter Right Now?
Advance Care Planning refers to structured conversations that help patients clarify and document their values, goals, and preferences for future medical care, particularly in the context of serious illness, chronic disease, or end-of-life decisions.
Medicare formally recognizes ACP through two CPT codes:
- 99497 – Advance care planning, including explanation and discussion of advance directives, first 30 minutes
- 99498 – Each additional 30 minutes, add-on code
These services may be provided face-to-face, can involve family members or surrogates, and, critically, can be billed on the same day as many E/M services, including Annual Wellness Visits (AWVs), when documentation supports a separate and identifiable service.
From a policy standpoint, ACP has been explicitly supported by CMS since 2016 and reinforced through quality initiatives emphasizing goal-concordant care and reduced unwanted utilization.
How Underused Are ACP Codes Across Medicare?
Despite broad eligibility, ACP remains dramatically underbilled.
Multiple national analyses show that only a small fraction of eligible Medicare beneficiaries receive billed ACP services:
- A study published in JAMA found that less than 7% of traditional Medicare beneficiaries had a billed ACP encounter over several years, despite far higher clinical need
- HHS Office of Inspector General reports consistently highlight underuse of preventive and care-coordination services, even when fully covered
The takeaway for leaders is simple:
ACP conversations are happening, but they are rarely structured, timed, documented, or coded in a way that allows them to be captured.
Why Are ACP Services Rarely Billed, Even When Care Is Delivered?
If you talk to clinicians, CDI teams, and coders, the reasons are remarkably consistent.
Is ACP “Hidden” Inside Other Visits?
Yes. ACP discussions frequently occur during:
- Annual Wellness Visits
- Chronic care follow-ups
- Post-hospitalization check-ins
- Conversations prompted by new diagnoses
But when time is not tracked separately and documentation does not clearly distinguish ACP from general counseling, the work becomes invisible from a coding perspective.
Are Documentation Standards Creating Friction?
Advance Care Planning documentation must clearly establish:
- Who participated (patient, family member, surrogate)
- What was discussed (values, goals, treatment preferences)
- Time spent (minimum 16 minutes for 99497)
- Whether advance directives were explained, completed, or updated
Without standardized templates or CDI reinforcement, providers often under-document, even when the clinical interaction fully qualifies.
Which Medicare Patients Are the Highest Value for ACP Services?
From both a clinical and operational lens, ACP should not be random.
High-value patient populations include:
- Patients with multiple chronic conditions
- Those with frequent ED visits or hospitalizations
- Early or moderate cognitive decline or dementia
- Advanced cardiac, pulmonary, renal, or oncologic disease
Studies consistently show that ACP is associated with:
- Improved patient satisfaction
- Reduced unwanted aggressive care
- Lower end-of-life utilization costs
For revenue cycle and CDI leaders, this means predictable, repeatable opportunities to embed ACP into care pathways.
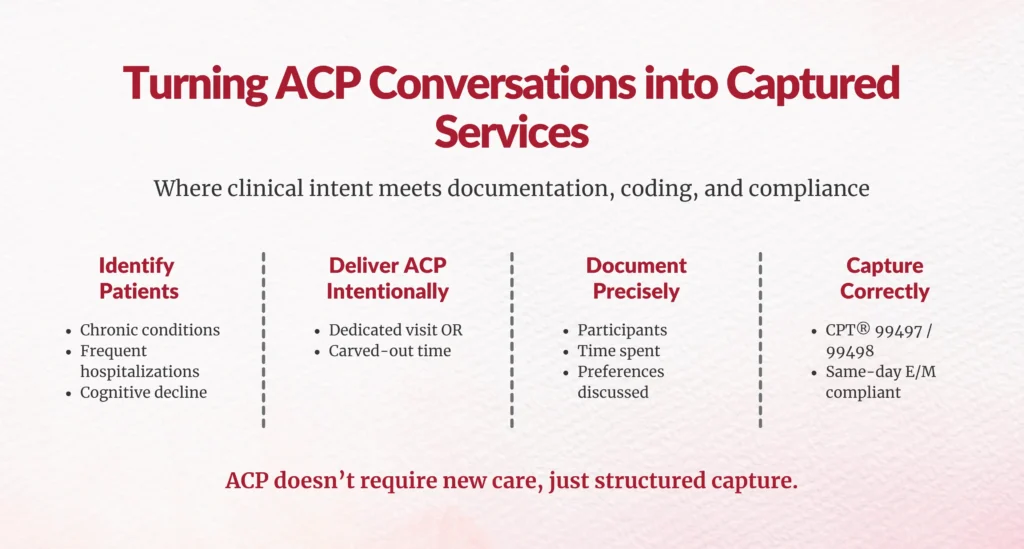
How Can Organizations Operationalize ACP Without Disrupting Workflow?
This is where leadership matters most.
Should ACP Be a Dedicated Visit or Integrated Service?
Best-performing organizations do one of two things:
- Schedule dedicated ACP visits for high-risk patients, or
- Intentionally carve out time during existing visits with explicit documentation and time tracking
Either approach works, as long as it is intentional.
What Role Do CDI, HIM, and RCM Teams Play?
Advance Care Planning is not “just a provider issue.”
- CDI teams ensure clinical intent and patient context are clearly documented
- HIM teams support compliant templates and retention of advance directive forms
- RCM teams validate modifier use, same-day billing rules, and payer policies
When these teams collaborate, ACP moves from “nice conversation” to captured clinical service.
How Does ACP Align With Quality, Compliance, and Financial Strategy?
Advance Care Planning sits at the intersection of:
- Patient-centered care
- Risk adjustment and care management
- Medicare compliance
- Sustainable revenue capture
- Legitimate reimbursement for work already being done
- Alignment with value-based care objectives
- Reduced downstream costs from unwanted or non-beneficial care
Importantly, ACP is not about chasing every code. It’s about stopping the systematic loss of high-value services that directly support patient outcomes.
What Is the Bigger Revenue Cycle Lesson Behind ACP?
Advance Care Planning is a case study in a broader issue facing Medicare-participating organizations.
Primary care and care teams deliver substantial non-procedural, cognitive, coordination-heavy work:
- Counseling
- Care planning
- Post-discharge follow-up
- Behavioral health support
Over the past decade, CMS has introduced CPT and HCPCS codes to recognize this work. On paper, they are covered. In practice, many remain underutilized.
For independent practices and health systems alike, this translates into:
- Missed revenue
- Underrepresentation of care complexity
- Misalignment between care delivered and care paid for

Are You Capturing ACP Services, or Giving Them Away?
So here’s the question you should be asking yourself as a leader:
Are ACP conversations happening in your organization, and if so, are they being captured in a compliant, consistent way?
If the answer is “we’re not sure,” that’s your opportunity.
Advance Care Planning doesn’t require new technology, radical staffing changes, or aggressive coding tactics. It requires:
- Awareness
- Workflow intention
- Documentation discipline
When done right, ACP supports patients, clinicians, and the financial health of your organization.
And perhaps most importantly, it ensures that care that truly matters, clinically and humanly, no longer goes unrecognized operationally.
FAQs
What is Advance Care Planning (ACP) and why does it matter for Medicare beneficiaries?
ACP involves structured discussions documenting patient values, goals, and preferences for future care, especially serious illness; supports goal-concordant care, reduces unwanted utilization.
Which Medicare CPT codes are used for Advance Care Planning, and what do they represent?
CPT 99497 (first 30 min face-to-face ACP) and 99498 (each additional 30 min); billable same-day as many E/M services.
Why are ACP services underused even when Medicare covers and reimburses them?
Discussions occur in AWVs/E/M but lack separate time tracking, structured documentation distinguishing ACP work.
Can ACP conversations be billed on the same day as an Annual Wellness Visit or other E/M services?
Yes, when documentation supports separate, identifiable service beyond E/M overlap.
What documentation requirements must be met to support ACP billing?
Must establish separate time spent, discussion content on advance directives, patient/family involvement, medical necessity.
Which patient populations offer the highest value for ACP services?
Medicare beneficiaries with serious/chronic illness, older adults, cognitive impairment, end-of-life needs.
How can clinical documentation integrity (CDI) teams support ACP capture and billing?
CDI reinforces templates, queries for separate time/content, ensures compliant distinction from other services.
What role do revenue cycle management teams play in ensuring ACP services are captured?
RCM standardizes workflows, verifies eligibility/coding, embeds ACP in billing rules/pathways.
How does ACP align with broader Medicare quality, compliance, and financial strategy goals?
Aligns with CMS quality initiatives for patient-centered care, adds reimbursable revenue from cognitive work.
What operational approaches help integrate ACP into routine workflows?
Dedicated visits or integrate into AWVs/hospital discharges using templates, team roles, intentional protocols.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.





