Concurrent Coding Services Built for Faster, Cleaner Reimbursement

Coding Challenges Emerging in High-Volume Care Environments
Retrospective coding and delayed documentation reviews create avoidable risk across revenue, compliance, and provider efficiency, especially in complex payor and value-based environments.

Why Chirok Health’s Concurrent Coding Services Deliver Results
Chirok Health’s concurrent coding model integrates certified coding and CDI expertise directly into live clinical workflows, ensuring documentation accuracy, coding precision, and payor alignment before claims are submitted.
How We Differ?
- Real-time review by certified coders for accurate diagnosis and procedure capture.
- Payor-aligned coding reduces denial risk and audit exposure.
- Timely, concise queries support providers without disrupting workflows.

AAPC/AHIMA/ACDIS
Certified professionals with deep experience in concurrent coding.

Specialty-Specific Expertise
Supporting concurrent coding across more than 30 clinical specialties.

Designed to Deliver ReDesigned to Support Multiple Payment Modelsal Value
Chirok Health’s Concurrent medical coding are built to support both fee-for-service and value-based care models.

Fee-for-Service
Ensure accurate E/M leveling, complete procedure capture, and compliant documentation before claims are submitted, reducing rework, denials, and billing delays.

Value-Based Care
Validate risk-adjustable diagnoses and clinical specificity in real time to support accurate HCC capture, quality reporting, and performance under value-based contracts.
Core Components of Our Concurrent Coding Services

Live Chart Review
Active review of clinical documentation as notes, orders, and results are created to identify gaps and coding opportunities before discharge.

Concurrent Code Assignment
Progressive assignment of diagnoses, procedures, and E/M levels during the encounter to minimize post-discharge coding delays.

Real-Time Provider Queries
Timely, focused queries issued while clinical context is fresh to clarify documentation and support accurate coding decisions.

Pre-Bill Coding Validation
Final review of codes and documentation prior to claim submission to ensure completeness, compliance, and clean billing.
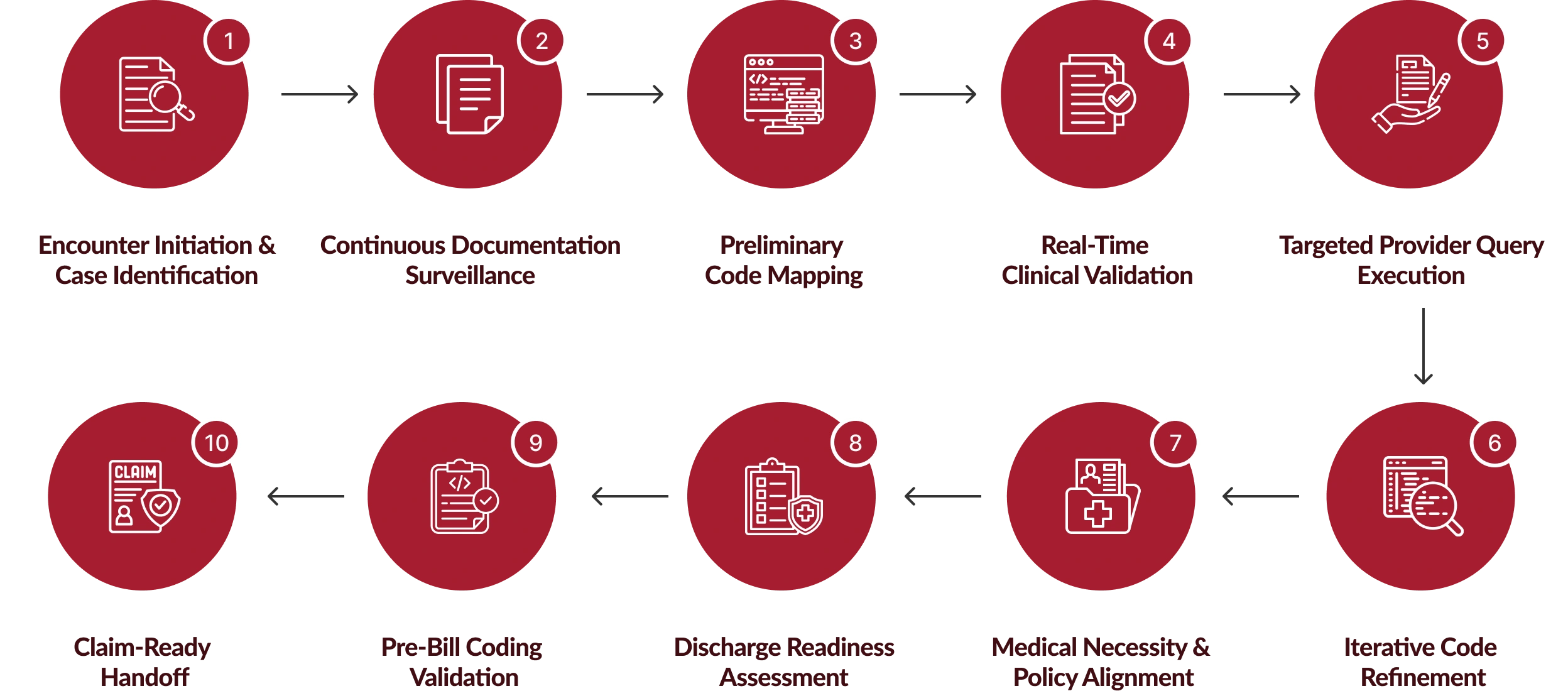
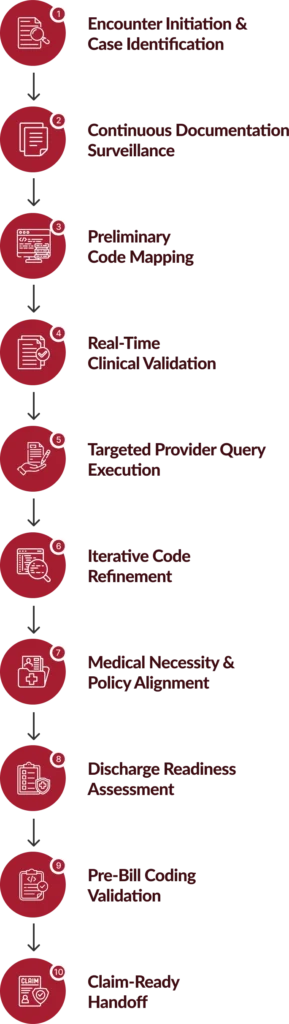
Comprehensive Concurrent Coding Services Workflow Built for Precision
As a concurrent coding company, Chirok Health follows a multi-stage, real-time workflow that operates alongside clinical care.
Results You Can Measure. Accuracy You Can Trust.
Chirok Health’s concurrent coding services are built to deliver fast ROI, sustained accuracy, and compliance confidence, without disrupting provider workflows or internal teams.

We guarantee 95%+ coding accuracy and a measurable ROI within 90 days, while mitigating compliance risk. Before you spend a dollar, we conduct a free clinical documentation and coding analysis to quantify missed revenue and improvement opportunities.
Coders communicate directly with providers through compliant, customized post-visit queries and monthly touchpoints, clarifying documentation without ever “teaching providers how to code.
Monthly dashboards give providers and leaders clear visibility into performance, trends, and how they compare to national benchmarks and peer organizations.
We connect you directly with current clients so you can validate results firsthand—our outcomes and testimonials speak for themselves.
We eliminate the tradeoff between Fee-for-Service and Value-Based Care by capturing both in real time, immediately after the visit and before the claim is submitted.
Impact of Our Concurrent Coding Services
Our concurrent coding services consistently deliver measurable improvements across productivity, risk adjustment, and revenue capture, validated through real-world performance outcomes.
Concurrent Coding Service That Works with Your EHR
Real-time coding and documentation review delivered directly within your existing clinical systems, no new tools, no workflow disruption.
Why It Matters
- Faster onboarding with minimal IT effort
- No disruption to provider documentation workflows
- Accurate, system-native coding and reporting






Who we serve
Supporting healthcare organizations with real-time concurrent coding services that improve documentation accuracy, reimbursement outcomes, and compliance at scale.

Hospitals
Supporting real-time documentation and coding accuracy across inpatient and outpatient encounters to reduce DNFB, denials, and post-discharge rework.

Community & Integrated Health Systemss
Delivering concurrent coding at scale across multiple facilities to standardize documentation, improve coding consistency, and protect system-wide revenue.

Academic Medical Centers
Balancing complex care delivery, teaching environments, and compliance requirements with real-time coding support during active encounters.

Medical Groups
Improving E/M and procedure capture through concurrent coding workflows that support providers without disrupting clinic operations.

ACOs & Risk-Bearing Organizations
Ensuring accurate, real-time capture of risk-adjustable diagnoses and clinical specificity to support performance under value-based contracts.
Value-Based Care RCM Staff Augmentation
Dedicated Chirok Health specialists extend your value-based care revenue cycle, supporting risk, quality, and contract performance across your organization.
Hear from Organizations We’ve Helped

“Chirok Health’s partnership has been invaluable, demonstrating remarkable adaptability in meeting our needs. Their comprehensive chart reviews ensure chronic conditions and potential health conditions are brought forth to our providers on time, enabling us to establish tailored care plans that truly meet our patients' needs.”


“Our Chirok partnership over the years has been amazing. The depth of knowledge and expertise is a given for Chirok, but their dedication to getting things right, working with us to improve each day, and the warmth of their people has set them apart. They are close colleagues and friends as well as coding partners, and we are very grateful for that.”


“The Chirok team consistently puts quality at the forefront, maintaining an unwavering dedication to compliance. Their commitment to accuracy is unparalleled, ensuring that our organization benefits from the highest standards without compromise. They are prompt, supportive, and a joy to work with. We are grateful for a partnership that blends excellence with efficiency.”

Get in Touch
Start Your Concurrent Coding Assessment
Whether you’re a hospital, health system, or medical group, Chirok Health helps you improve coding accuracy, reduce denials, and accelerate reimbursement through real-time concurrent coding services. Complete the form to start a focused conversation.
Contact Form
Got Questions?
We’ve Got Answers!
In complex hospital environments, accuracy issues are usually caused by documentation timing gaps, specialty variation, and downstream rework, not coder skill. Concurrent coding closes these gaps by addressing issues while the encounter is still active, when clarification is fastest and most reliable.
Concurrent coding helps revenue cycle leaders improve first-pass claim acceptance, DNFB performance, and cash predictability by reducing late-stage corrections, post-discharge queries, and avoidable denials.
Yes. Concurrent coding is especially effective in large, multi-specialty, high-volume organizations where documentation complexity and provider variation make post-discharge coding inefficient and risky.
Concurrent coding works alongside CDI by reinforcing documentation specificity and clinical clarity in real time, reducing retrospective CDI workload and improving provider adoption without duplicating efforts.
Yes. Chirok Health designs concurrent coding workflows to minimize provider interruptions, using structured queries and clear escalation paths that respect clinical priorities and reduce administrative burden.
By identifying and resolving documentation and coding gaps early, concurrent coding ensures claims are accurate, supported, and defensible, reducing exposure during internal audits, payer reviews, and regulatory scrutiny.
Concurrent coding delivers the highest impact in high-acuity and high-volume service lines such as inpatient, emergency departments, surgical services, and specialty care where documentation and coding complexity is highest.
Yes. Concurrent coding can be engaged independently or as part of a broader RCM or CDI strategy, including auditing and ongoing compliance monitoring based on organizational needs.
Most organizations begin seeing improvements within 30–60 days, including faster coding turnaround, fewer post-discharge queries, and improved documentation consistency across providers.
Beyond immediate gains, concurrent coding provides insights into documentation trends, provider variation, and systemic gaps, helping leadership strengthen governance, education, and compliance programs over time.



