HEDIS Reporting and Documentation Last Minute Gaps That Impact Quality Scores
Why Do Last-Minute HEDIS Documentation Gaps Still Derail Quality Scores?
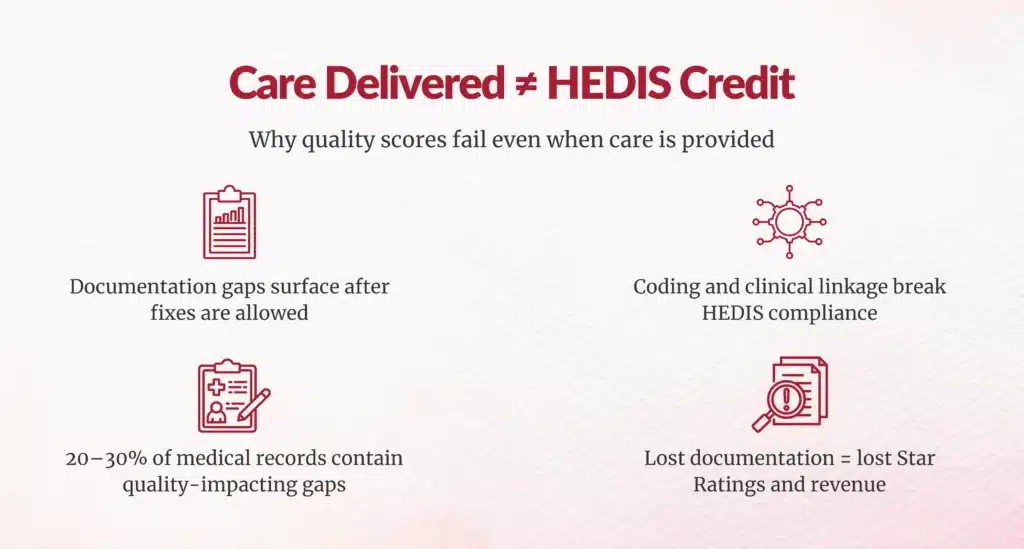
If you’re leading CDI, HIM, or Revenue Cycle today, you already know the uncomfortable truth: most HEDIS failures don’t occur because care wasn’t delivered; they occur because it wasn’t documented, coded, or linked correctly in time.
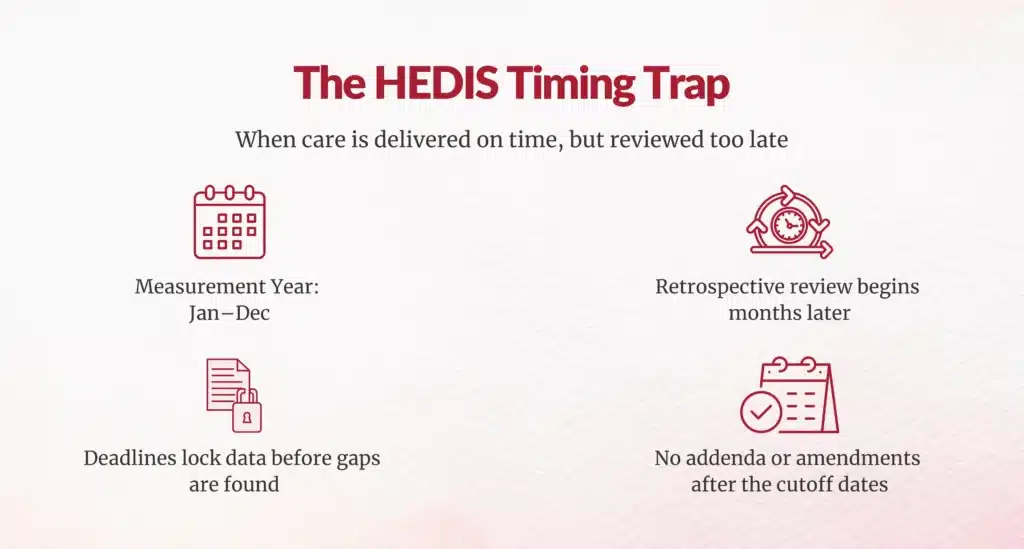
Each measurement year, healthcare organizations face the same pattern. As reporting deadlines approach, teams scramble to retrieve charts, validate services, and respond to audit requests, only to discover documentation gaps that are no longer correctable. These gaps directly lower quality scores, Star Ratings, and financial performance.
According to AHIMA, 20–30% of medical records contain documentation gaps that negatively impact quality reporting and reimbursement.
What Makes HEDIS Timing So Unforgiving?
How Does the HEDIS Measurement Year Create Structural Risk?
Key NCQA deadlines include:
- January 30, 2026 – Roadmap submission and end of nonstandard supplemental data collection
- February 27, 2026 – Final nonstandard supplemental data amendments
- May 22, 2026 – Medical record review validation completion
- June 15, 2026 (9 PM ET) – Final audited submission
(Source: NCQA HEDIS Technical Specifications)
Why Are Documentation Errors Often Discovered Too Late?
Services rendered early in the year may not be reviewed until April or May of the following year. At that point, coding corrections, documentation addenda, or supplemental data amendments are no longer allowed, leaving organizations locked into lost quality credit.
What Are the Root Causes Behind Last-Minute Documentation Gaps?
How Do Fragmented Data Systems Hide Care Gaps?
Healthcare data remains siloed across:
- EHR platforms
- Claims and billing systems
- Laboratory portals
- Care management tools
When systems fail to integrate, delivered care does not translate into HEDIS-compliant evidence. NCQA audits consistently cite data fragmentation as a top contributor to failed measures.
Why Does Documentation Specificity Matter More Than Intent?
HEDIS requires explicit clinical proof, not implied care.
What Documentation Elements Are Commonly Missing?
- MEAT criteria (Monitoring, Evaluation, Assessment, Treatment)
- Clear clinical linkage between related conditions
- ICD-10 codes at the highest documented specificity
For example, documenting “diabetes” without type or control status can invalidate the entire measure, even when care was appropriate.
How Does Provider Alert Fatigue Contribute to Gaps?
Providers face constant alerts across multiple quality programs. Preventive and quality documentation often loses priority to acute care needs, especially late in the year. This results in deferred screenings and incomplete documentation that surface only during retrospective review.
Which HEDIS Measures Are Most Vulnerable to Documentation Failure?
Why Do Diabetes Comprehensive Care Measures Fail So Often?
Diabetes measures are among the most heavily weighted HEDIS metrics.
Common Diabetes Documentation Failures
- Missing HbA1c numeric values
- Retinal exam documentation lacking exam type or provider specialty
- Blood pressure documented without numeric readings
- Kidney screening documented as ordered, not completed
(Source: NCQA Diabetes Measures)
Why Do Functional Status and Pain Assessment Measures Break Down?
These measures require standardized tools, not narrative notes.
Typical Failure Patterns
- ADLs and IADLs not documented using approved instruments
- Pain assessments lacking standardized severity scoring
Many EHRs lack templates that support this level of structured documentation.
What Breaks Medication Review Compliance?
Medication review requires:
- A complete medication list (Rx, OTC, supplements)
- Same-day reconciliation
- Review by a qualified provider
Documentation completed days later or by unqualified staff fails HEDIS criteria.
Why Does Supplemental Data Become a Last-Minute Bottleneck?
How Do Nonstandard Supplemental Data Deadlines Create Risk?
Nonstandard supplemental data must be finalized by January 30, 2026, with no exceptions. Documentation must prove services were delivered, not merely ordered.
How Do Medical Record Retrieval Delays Compound Losses?
Late chart retrieval increases error rates and missed deadlines. HFMA reports organizations can lose 20–30% of potential quality value due to retrieval delays alone.
How Do Documentation Gaps Impact Revenue Beyond HEDIS?
What Is the Financial Cost of Documentation Failure?
- Claim denial rates: 11–20%
- Cost per denied claim: $25–$118
- 65% of denied claims are never resubmitted
Documentation failures compound losses across quality scores, reimbursement, and cash flow.
What Do HEDIS Audits Consistently Identify as Preventable Errors?
Common NCQA Audit Findings
- Claims without supporting clinical documentation
- Missing authorized source records
- Untimely submissions lacking clinical context
- Inconsistent data across systems
In most cases, the care occurred, but the proof failed.
Why Do Organizational Workflows Make Last-Minute Chaos Inevitable?
Lack of Real-Time Visibility
Without in-year dashboards, gaps remain invisible until retrospective review.
Provider Coordination Failures
Year-end outreach competes with clinical priorities and produces poor response rates.
Insufficient Training
Staff often don’t understand how specific language affects HEDIS compliance until audits begin.
Can Technology Prevent Last-Minute HEDIS Gaps?
How Do AI and Automation Change Outcomes?
Organizations using NLP and AI-driven abstraction report:
- 75% efficiency gains
- 95%+ accuracy compared to manual review
These tools identify gaps during the measurement year, not after it ends.






What Strategic Shifts Actually Close HEDIS Gaps for Good?
Why Is Year-Round Gap Management Essential?
Leading organizations move from reactive “chase-and-close” models to proactive, continuous monitoring.
How Does Unified Data Architecture Reduce Risk?
Integrating EHR, claims, labs, and care management data enables near–real-time visibility into measure performance.
Why Does Continuous Education Matter?
Ongoing provider and staff education ensures everyone understands what HEDIS requires before audits begin.
What Is the Bottom Line for HIM and Revenue Cycle Leaders?
Most HEDIS quality losses are preventable. They stem from documentation, timing, and system failures, not a lack of care delivery.
If your organization is still fighting HEDIS fires in Q2, the problem didn’t start in Q2.
It started quietly in January, and that’s where sustainable improvement must begin.
FAQs
Why do HEDIS documentation gaps still occur even when care was appropriately delivered?
Gaps arise from siloed data systems (EHR/claims/labs), missing specificity (MEAT criteria, ICD-10 detail), provider alert fatigue prioritizing acute care over preventive documentation.
How does the HEDIS measurement year structure create documentation risk?
Care Jan-Dec reviewed April-May next year; deadlines (Jan 30 roadmap, June 15 final) lock uncorrectable gaps from early-year services discovered too late.
Which specific HEDIS measures are most vulnerable to documentation errors?
Diabetes care (missing HbA1c values, retinal exams), functional status/pain assessments (no standardized tools), medication reviews (incomplete lists/reconciliation).
What documentation elements does NCQA require for HEDIS compliance?
MEAT criteria (Monitor/Evaluate/Assess/Treat), highest ICD-10 specificity, numeric values (HbA1c/BP), standardized tools, clinical linkage/proof of delivery.
How does fragmented data across EHR, claims, and labs contribute to HEDIS gaps?
Siloed systems prevent integrated visibility; delivered care fails to appear as HEDIS evidence, cited as top NCQA audit failure contributor.
Why does provider alert fatigue worsen HEDIS documentation performance?
Constant quality alerts compete with acute priorities; preventive documentation deferred, surfacing as retrospective gaps late in measurement year.
Can organizations fix HEDIS documentation gaps after the annual reporting deadline?
No, nonstandard supplemental data finalizes Jan 30, 2026; medical record validation ends May 22; late gaps remain uncorrectable post-deadlines.
How should healthcare leaders improve HEDIS documentation year-round?
Implement real-time dashboards, unified data architecture, continuous provider education, proactive gap monitoring vs. reactive year-end chases.
What role does AI and automation play in preventing HEDIS documentation failures?
NLP/AI abstraction yields 75% efficiency gains, 95%+ accuracy, identifies gaps during measurement year for timely closure.
How do HEDIS documentation gaps impact financial performance beyond quality scores?
Drive 11–20% claim denials ($25–$118 rework each), 65% never resubmitted, lowering Star Ratings/reimbursements.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.





