AI in Revenue Cycle Management: What’s Actually Working vs. What’s the Hype for 2026
Is AI in Revenue Cycle Management Delivering Real ROI or Just Hype for 2026?
Artificial intelligence hit peak hype in healthcare this 2026. Every startup claims to be “AI-powered,” legacy vendors tout “AI suites,” and machine learning is pitched as the silver bullet for Revenue Cycle Management (RCM). The reality? Some capabilities are proven and delivering measurable ROI; others are promising but nascent; and many remain marketing fluff.

This month’s Revenue Cycle Report is dedicated to cutting through the noise so you can understand AI’s true potential in RCM and where it delivers impact you can measure.
What’s the Bottom Line Right Now: Is AI Delivering Real Results in RCM?
Yes, but selectively.
Across billing, claims management, denials, and patient engagement, AI is already driving operational gains when applied to the right problems with strong data governance and human oversight. These real-world wins include:
- Faster denial appeal generation with clinically calibrated generative AI
- Automated document classification and claims status tracking
- Predictive scoring that highlights high-risk accounts
- Rule-based automation handling structured tasks with precision
These capabilities aren’t “fully autonomous robots”, they augment workflows and reduce manual effort. AI excels where data quality is high, outcomes are measurable, and feedback loops exist.
What Types of AI Are Actually Working in RCM Today?
Are Rule-Based Automations Still Relevant?
Absolutely, and extremely effective.
Deterministic, rules-based automation (e.g., robotic process automation or RPA) reliably handles structured, repetitive work such as appointment reminders, eligibility checks, and claims follow-ups. It’s mature technology that removes human drudge work and improves consistency. But it’s brittle, it breaks when exceptions occur, and cannot adapt without human intervention.
Think of RPA as the foundation: reliable, cost-reducing, and predictable, but not “intelligent.”
How About Natural Language Processing (NLP) and Classic Machine Learning?
These cognitive technologies are proven and expanding.
- NLP accurately classifies unstructured text in notes, appeal drafts, and correspondence.
- Supervised machine learning helps predict denials and prioritize accounts receivable.
These tools require curated datasets and good labels, but they’re delivering measurable gains when integrated into workflows. Hospitals and health systems are increasingly adopting them to automate document handling and boost accuracy.
Example: Predictive models can score accounts for AR prioritization, leading to better cash collections and fewer days in AR.
Is Generative AI Like ChatGPT Actually Useful in RCM?
Yes, but within guardrails.
Generative models can draft appeal letters, summarize clinical documentation, and create financial communications. They reduce manual writing time and help standardize language across teams.
However, without strong clinical oversight, governance, and quality checks, these models can generate inaccurate or non-compliant content, which is unacceptable in healthcare billing and compliance.
Generative AI is useful as a co-pilot, not a replacement for expert reviewers.
What’s Next: Emerging AI That’s Close to Real Impact?
Can AI Orchestrate End-to-End Workflows Autonomously?
This is where Agentic AI comes in.
Agentic AI systems reason across steps and can act semi-independently, routing claims, adjusting workflows, and even correcting errors. These capabilities are promising, but still fragile in real practice due to:
- payer rule changes
- hospital-specific nuances
- missing documentation
They perform beautifully in controlled pilots but often struggle in broader deployment. Agentic AI is the “next frontier,” but should be deployed cautiously with robust human oversight.
Is Predictive Analytics Evolving Beyond Today’s Models?
Yes, next-gen predictive analytics will span multiple RCM domains, using richer datasets and more sophisticated learning techniques. Still, the success of these systems depends on:
- data completeness
- model calibration
- continuous feedback loops
Without those, predictive models can underperform or misclassify risk, resulting in lost revenue or compliance issues.
What’s Still Hype and Not Ready for Production Use?
Will AI Replace Human Revenue Cycle Teams?
Absolutely not;
A fully autonomous, self-learning AI that manages your entire revenue cycle without human intervention is an overstatement and a compliance risk. Healthcare RCM requires nuanced judgment, exception handling, and regulatory awareness that only trained humans currently provide.
Human-in-the-loop governance remains essential. AI augments decisions; humans own outcomes.
Are Vendor “AI Suites” All Created Equal?
Unfortunately, no.
Many vendors label even basic automation and analytics as “AI” to ride the hype wave. When evaluating solutions, ask for transparency on:
- model type (NLP? supervised learning? deep learning?)
- training data sources
- real performance metrics
- governance and audit processes
If a vendor can’t explain why their AI works in your context, treat the claim with skepticism.


What Questions Should You Ask Vendors About AI Claims?
What AI Technology Are You Actually Using?
Different AI technologies have different maturity and risk profiles. Knowing the type helps you match the tech to your problem:
- Document classification → NLP
- Denial prediction → Supervised ML
- Radiology interpretation → Deep learning
- Conversational agents → Generative AI + governance
How Do You Govern and Validate AI Outputs?
AI can be powerful but prone to drift and bias. Ask vendors:
- How do they monitor model performance over time?
- What guardrails ensure compliant outputs?
- Is there a human review layer?
Without strong governance, models may degrade or produce risky recommendations.
What ROI Are Organizations Seeing with AI in RCM?
Healthcare leaders are beginning to quantify impact:
- Faster appeal submission with generative AI
- Higher AR cash collections with predictive prioritization
- Lower abandonment rates with intelligent voice agents
According to industry analyses, AI adoption in healthcare administrative workflows has shown meaningful reductions in cost and time while increasing accuracy. For example, a recent study found that automating administrative tasks with AI can reduce labor costs by up to 40% in some areas while improving cycle times.
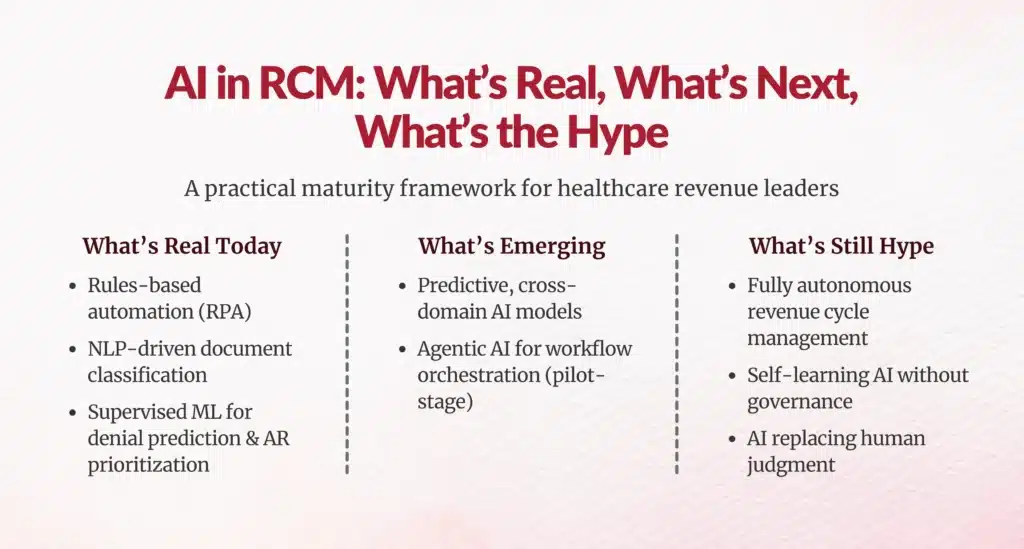
Final Verdict: What’s Real vs. Hype for 2026
Here’s a simple framework to assess AI claims in RCM:
| Capability | Status in 2026 | Why |
|---|---|---|
| Rules-based automation | Real | Mature and reliable |
| NLP & classic ML | Real and growing | Effective with good data |
| Generative AI | Useful with guardrails | Great co-pilot, not autonomous |
| Predictive RCM models | Next wave | Powerful with governance |
| Agentic AI orchestration | Emerging | Promising, not yet robust |
| Fully autonomous RCM | Hype | Compliance risk |
Bottom Line to Leaders
AI in RCM isn’t a magic switch; it’s a toolset. The real winners in 2026 will be organizations that:
- Understand where specific AI technologies create value
- Build high-quality data foundations
- Implement governance and safety processes
- Keep humans engaged in oversight and decision-making
AI is transformational when applied thoughtfully, boosting efficiency, reducing errors, and enabling your teams to focus on high-value work. But it’s not one monolithic innovation; it’s a continuum of capabilities with different maturity levels.
By cutting through the hype, asking the right questions, and investing in data and governance, RCM leaders can unlock real impact from AI in 2026.
FAQs
What AI technologies are actually delivering measurable value in revenue cycle management as of 2026?
Rule-based automation (RPA), NLP for document processing/denials, classic ML for AR prioritization/coding all deliver proven ROI with 40% labor reductions, faster collections.
How does rule-based automation differ from AI in RCM, and why is it still important?
RPA handles structured/repetitive tasks reliably (eligibility, reminders) unlike adaptive AI; remains foundational for consistency, cost reduction despite brittleness on exceptions.
What role do NLP and classic machine learning play in healthcare revenue cycle workflows?
NLP automates document handling, denial prediction; ML prioritizes AR accounts, improves coding accuracy using curated datasets and measurable feedback loops.
Is generative AI like ChatGPT reliable for drafting denial appeals and other RCM tasks?
Useful as co-pilot for drafting appeals/summaries with guardrails, clinical oversight; risks inaccurate/non-compliant content without quality checks.
What is agentic AI, and why is it considered the next frontier in RCM?
Agentic AI reasons across workflows, routes claims semi-autonomously; promising for orchestration but fragile needing human oversight in production.
Why is human oversight essential even when AI technologies are used in revenue cycle management?
AI lacks nuanced judgment, exception handling, regulatory awareness; humans ensure compliance, validate outputs, own outcomes in healthcare RCM.
What data quality and governance practices are needed for successful AI adoption in RCM?
Curated datasets, strong labels, explainability, validation, feedback loops, human-in-loop governance prevent drift, bias, compliance risks.
What questions should healthcare leaders ask vendors about their AI claims in RCM?
Ask AI type/maturity, governance/validation methods, model explainability, data sources, performance metrics in your context.
How can healthcare organizations measure the ROI of AI tools in their revenue cycle processes?
Track labor cost reductions (up to 40%), denial rates, days in AR, collection speeds, first-pass acceptance rates.
Which AI capabilities are still considered hype rather than proven solutions for RCM?
Fully autonomous RCM replacing humans, unproven vendor "AI suites" without transparency remain hype and compliance risks.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.





