RADV Audit Risk Surge November 2025 Data Shows 30 % Increase
Why Are RADV Audits Surging by 30% in Late 2025?
In November 2025, healthcare leaders are facing a significant surge in risk adjustment data validation (RADV) audit activity, approximately 30 % more notices, requests, and regulatory pressure compared with early 2025 baselines. This escalation reflects a systemic shift from occasional, targeted reviews to routine, comprehensive oversight by CMS and fuels urgency for leaders in revenue cycle, HIM, and CDI to act now.

This surge hasn’t happened in a vacuum; it follows CMS’s massive overhaul of the RADV program, expanding audit volume, sample sizes, and enforcement intensity. The result? Greater financial exposure for Medicare Advantage plans, and downstream operational impacts for provider organizations supporting risk adjustment documentation.
What Is a RADV Audit and Why Is It Suddenly a Top Risk in 2025?
In plain terms, RADV audits verify that diagnoses used to calculate risk-adjusted payments — the Hierarchical Condition Categories (HCCs) reported by Medicare Advantage Organizations (MAOs), are supported by clinical documentation in medical records. If CMS finds unsupported conditions, it can claw back millions in overpayments via extrapolation across entire enrollee populations.
Why RADV matters now:
- It ensures the integrity of Medicare Advantage risk adjustment, a $450 + billion annual program.
- Unsupported diagnoses can trigger extrapolated repayment, multiplying penalty amounts far beyond the sampled charts.
- RADV shifts risk from “rare compliance event” to continuous regulatory pressure, especially with CMS’s 2025 audit expansion.
Why Did RADV Audit Risks Increase in 2025?
Has CMS Really Expanded RADV Audits That Much?
Yes. In 2025, CMS announced an aggressive national RADV audit expansion:
- Audit universe expanded from ~60 Medicare Advantage contracts annually to all eligible MA plans (~550+).
- Medical record sample sizes increased from ~35 member charts per plan up to 200 charts annually, depending on plan size.
- CMS grew RADV medical coding reviewers from ~40 to about 2,000 coders by late 2025.
This dramatic scaling alone drives a 30 + % increase in RADV notices and audit activity in late 2025 compared to 2024/early 2025 levels, even before factoring in providers’ growing backlog of document requests and contract-specific outreach.
Bottom line: RADV isn’t “once-in-a-while” anymore; it’s annual, routine, and comprehensive.
What’s Driving This Enforcement Shift?
Is CMS Just Targeting Plans for Penalties?
Not exactly, CMS’s stated intent is to protect public funds by validating that diagnoses reported for risk-adjusted payments are supported in medical records.
However, broader audit escalation reflects:
- Growing concerns about overpayments due to unsupported diagnosis coding.
- Building backlog, CMS aims to finish audits for Payment Years 2018–2024 by early 2026.
- Legislative and public pressure to improve accuracy and crack down on improper Medicare spending.
This means RADV is now part of the standard compliance environment, not a niche audit risk.
What Does the 30 % Increase in RADV Audit Risk Mean for Your Organization?
Operational and Financial Impacts
1. Increased Documentation Requests
You & your providers will see more medical record requests, including older encounters from multiple care settings, to support risk adjustment diagnoses.
2. Bigger Extrapolation Exposure:
Errors found in even a small sample can be extrapolated across your full Medicare Advantage enrollee population, turning hundreds or thousands of dollars of issues into multimillion-dollar liabilities.
3. Coding & Clinical Documentation Risks:
Unsupported or poorly documented diagnoses may trigger:
- Payment clawbacks
- Increased provider appeals workload
- Impact to MA plan star ratings and quality measures
- Strained provider and plan relationships
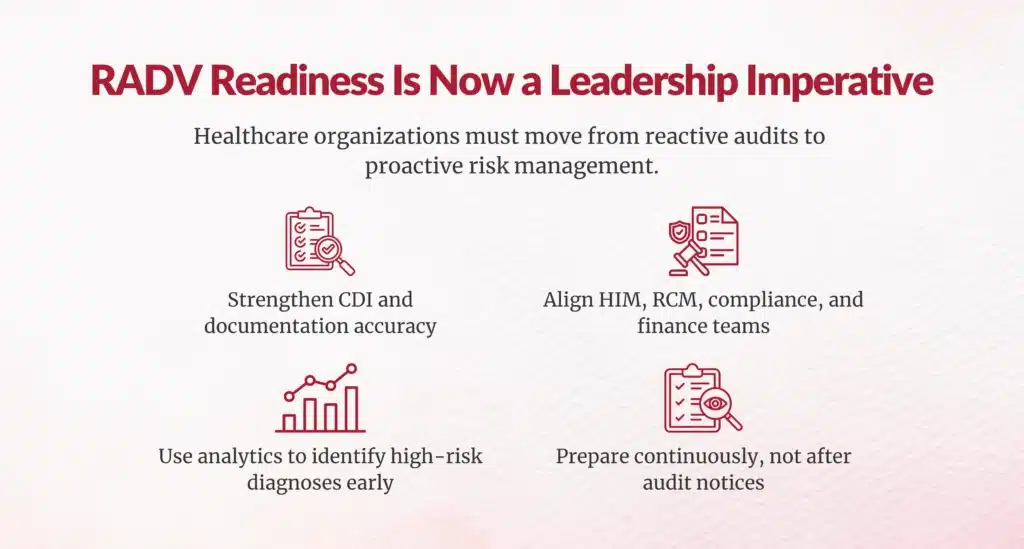
How Should Healthcare Leaders Respond?
If you’re leading HIM, CDI, RCM, or financial strategy, this risk surge means shifting from reactive reporting to proactive RADV readiness.
1. Embed RADV Readiness Across Teams
Break silos:
- Align CDI, coding, RCM, quality, and compliance teams.
- Build agreed workflows for documentation, coding, and audit responses.
2. Strengthen Clinical Documentation (CDI) and Coding
Ensure diagnoses meet MEAT criteria, Monitored, Evaluated, Assessed, Treated, which is the key standard CMS reviewers look for in RADV audits.
Offer clinician education and CDS templates that specifically:
- Link conditions to clinical encounters
- Document severity, treatment, and progression
- Minimize problem-list only documentation
3. Use Data Analytics and AI Tools
AI-assisted chart review and risk-adjustment analytics can:
- Flag unsupported HCCs
- Prioritize high-risk records for review
- Improve first-pass accuracy
This transforms RADV work from manual checklists into predictive compliance workflows.
4. Conduct Routine Internal RADV Simulations
Implement internal RADV-style audits quarterly:
- Select representative chart samples
- Assess coding, documentation, and support evidence
- Track error rates across your MA populations
This “practice audit” environment prepares teams for real CMS requests, reducing surprise exposures and unplanned financial hits.
5. Improve Documentation Retrieval Infrastructure
Audit readiness is as much logistical as analytical. Invest in:
- Electronic medical record search tools
- Provider attestation systems
- Centralized chart retrieval and tracking
This reduces pain and turnaround time when CMS or plans request records.
What Should CFOs and VPs of RCM Prioritize Now?
Quantify your exposure:
- Estimate the potential financial impact of RADV extrapolation.
- Model sensitivity on error rates and sample sizes.
Invest in pre-audit readiness:
Funding proactive documentation improvement, analytics, and education now is a fraction of the cost of responding to extrapolated findings later.
Build cross-functional governance:
Create a RADV steering committee involving CDI, coding, HIM, compliance, and analytics, measured on error reduction KPIs.
Monitor regulation continually:
CMS’s audit strategy continues evolving, including legal challenges affecting extrapolation rules, so staying current on regulatory updates is essential for risk mitigation.





RADV Is No Longer Optional Compliance, It’s Strategic Risk Management
The 30 % surge in RADV audit risk in November 2025 isn’t a one-off. It’s the result of CMS’s systemic shift toward broader, deeper, and more frequent audit activity, designed to protect the Medicare Advantage program and federal funds.
For HIM Directors, CDI leaders, RCM Directors, and financial executives, this means:
- RADV readiness must be woven into everyday workflows.
- Documentation quality isn’t just compliance; it’s revenue protection.
- Advanced analytics and integrated cross-disciplinary collaboration aren’t optional anymore.
If you haven’t already, now is the time to assess, plan, and operationalize RADV audit readiness across your organization, because the risk is here to stay.
FAQs
What is RADV and why were audits increased in 2025?
RADV (Risk Adjustment Data Validation) verifies HCC diagnoses support risk-adjusted MA payments via medical records; 30% audit surge from CMS national expansion, annual contract audits through 2026.
How does a 30% RADV audit surge impact healthcare revenue?
Unsupported diagnoses trigger extrapolated overpayment clawbacks across entire enrollee populations, creating millions in financial penalties for MA plans/providers.
What documentation elements are most frequently targeted in RADV audits?
Face-to-face provider encounters, definitive diagnoses (no probable/suspected), MEAT criteria (Monitor/Evaluate/Assess/Treat), signed attestations within 6 months.
How can health systems assess their RADV risk exposure?
Review HCC coding patterns, outlier RAF scores, documentation completeness, audit backlog; benchmark against peer contracts for CMS selection risk.
What proactive audit readiness steps reduce RADV risk?
Validate HCCs annually, strengthen clinical documentation, implement MEAT compliance, prepare record retrieval processes before notices arrive.
How should CDI and coding teams collaborate to defend against RADV audits?
CDI ensures clinical validation/MEAT support; coding verifies HCC accuracy; joint reviews address documentation gaps proactively.
What performance metrics signal a RADV risk before an audit notice arrives?
High RAF outliers, unsupported HCC ratios, documentation gap rates, query response trends, peer benchmarking variances.
Can analytics tools predict which records are RADV vulnerable?
Yes, NLP/HCC validation analytics identify weak documentation, missing MEAT, high-risk diagnoses before submission.
What payer behaviors are driving the recent RADV activity surge?
CMS shifts to routine annual audits (PY2018-2024 by 2026), responds to OIG/GAO improper payment concerns, protects federal MA funds.
How does RADV differ from other CMS audits in scope and documentation demand?
RADV targets HCC/RAF validation across entire MA contracts with extrapolation; demands MEAT-proof clinical records vs. procedural coding focus.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.





