31 % of Coding Staff Consider Leaving What Healthcare Systems Are Doing to Retain Talent
If you lead HIM or the revenue cycle, you’re already feeling the pressure: rising workloads, widening talent gaps, and increasingly unstable staffing pipelines. The headline number, 31% of healthcare workers considering leaving, comes from a McKinsey & Company survey on the nursing workforce, where nearly one-third of nurses reported an intent to leave direct patient care within a year.
Even though this specific metric reflects nursing, the drivers behind that intention burnout, low recognition, unsafe environments, and stagnant compensation mirror what’s happening in medical coding and HIM.
Here’s the reality you already know but may not have data on:
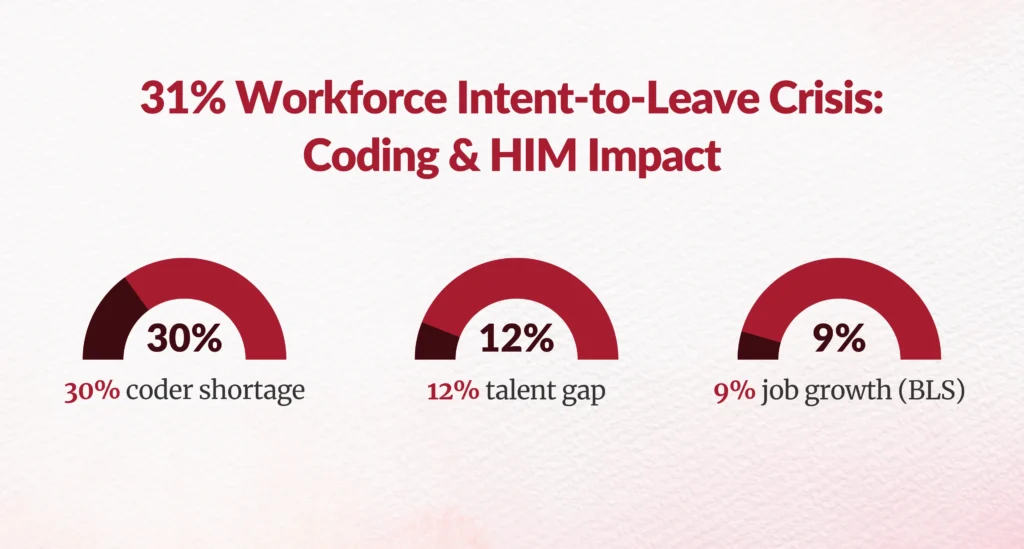
- The U.S. faces a 30% shortage of certified medical coders.
- The Bureau of Labor Statistics projects 9% job growth for medical records specialists through 2033.
- AAPC estimates a 12% nationwide coding talent gap in 2025.
So yes the 31% figure isn’t just a number. It’s a warning signal for every revenue cycle leader.
The pressing question is: What can you do about it?
Let’s walk through what healthcare systems are actually doing successfully to retain coding and HIM staff.
What Are the Primary Reasons Coding and HIM Professionals Are Leaving?
Is Compensation Still the Biggest Driver?
Short answer: Yes.
According to AHIMA and NORC research, 47% of HIM professionals cite low compensation as their top reason for leaving.
Coders specifically report:
- Wage stagnation
- Limited advancement pathways
- Salary compression between new and tenured team members
You already know compensation doesn’t solve everything, but it absolutely sets the baseline.
What role does real-time physician support play?
A massive one. Workloads have increased due to:
- Rising complexity in HCC, risk adjustment, and specialty coding
- Backlogs from staffing shortages
- Expanded documentation requirements
- Pressure to reduce DNFB and accelerate TAT
- Remote work fatigue
McKinsey reports that nurses leaving direct care cite:
- Feeling undervalued
- Unmanageable workloads
- Not enough support
These apply directly to your coding teams.
Are Safety and Work Environment Factors Still Relevant for Coders?
Surprisingly, yes.
While coders aren’t facing bedside physical risks, they report:
- Psychological stress
- Isolation in remote roles
- Lack of structured team suppor
- Poor managerial communication
This “silent strain” contributes heavily to turnover.
What Are Healthcare Systems Actually Doing to Retain Coding and HIM Talent?
Below are evidence-based strategies implemented by major health systems and how you can adopt them.
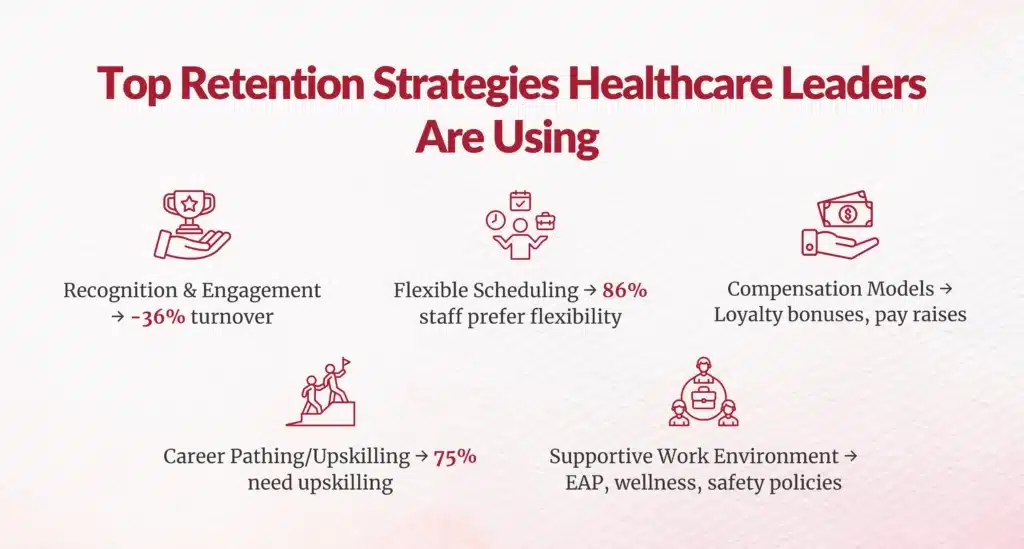
How Are Organizations Improving Recognition and Meaningful Engagement?
Are simple recognition programs enough?
Not anymore. But structured recognition is making a measurable difference:
Orange Coast Medical Center implemented Laudio, a workforce engagement platform. With just one meaningful interaction per month per employee, the system reduced turnover by 36%.
Orlando VA Medical Center created Employee Well-being Centers quiet rooms with VR, aromatherapy, and rest spaces. Result? Increased retention and higher wellness engagement scores.
Actionable strategy for HIM leaders:
Start monthly recognition touchpoints, track engagement, and celebrate coder accuracy wins, TAT improvements, and productivity milestones.
Is Flexibility Still the #1 Factor in Retention?
Absolutely 86% of healthcare staff say flexibility is a major reason they stay (McKinsey).
For coders specifically, remote work is no longer a perk it’s an expectation.
Leading examples:
- Mercy Health created “Mercy Works on Demand,” hiring 1,100 gig nurses with flexible scheduling.
- Henry Ford Health brought back 25% of nurses who left by offering mix-and-match shifts.
- Trinity Health deployed virtual-care roles systemwide.
Your actionable opportunity:
Offer coders:
- Split shifts (e.g., 6–10 AM + 6–9 PM)
- Seasonal or project-based roles
- Weekend-only coding pools
- “Anywhere workforce” remote-first contracts
What Compensation Models Are Improving Retention?
Yes, organizations are increasing salaries. But the most successful use strategic compensation:
- Loyalty bonuses (stay 6–12 months to incentive payout)
- Milestone bonuses (credential advancement, audit scores, accuracy)
- Certification reimbursement
- Tuition and student loan support
According to NSI’s 2025 report, hospitals with strong workplace cultures pay 11% less to retain talent because people stay for the environment, not just the paycheck.
Are Career Growth and Upskilling Critical for Coders?
More than ever.
AHIMA finds 75% of HIM professionals need upskilling due to rapid tech evolution EHR changes, CAC tools, AI-assisted coding, and regulatory shifts.
Examples:
- Children’s Hospital of Philadelphia (CHOP) replaced their advancement model with the PEAK program personalized development tracks.
- Dignity Health partners with higher education systems to offer online degrees for coding and HIM staff.
Your move:
Create micro-promotion tracks like:
- Senior Coder to Coding Quality Reviewer
- Documentation Integrity Track to CDI Analyst
- Project Lead Track to EHR Template Advisor
How Are Organizations Improving Work Environment and Safety for HIM Teams?
Does psychological safety matter for remote HIM teams?
More than most leaders realize.
UMass Memorial’s patient and visitor code of conduct improved staff confidence and safety after collecting 56,000 signed agreements in its first weeks.
For HIM, psychological safety means:
- Healthy communication norms
- Regular 1:1 check-ins
- Clear workload distribution
- Transparent expectations
- Burnout monitoring
- Access to EAPs and mental health support
Wellness initiatives (meditation, fitness, micro-breaks) are also now standard.
Does Outsourcing Really Help With Coding Retention?
Sometimes the best retention strategy is reducing the burden altogether.
Case studies:
- Hospitals partnering with 3M and others reduced backlogs and improved quality without overwhelming existing teams.
- Organizations working with Gebbs achieved:
- 96% HIM accuracy
- 85% reduction in TAT
- 50% decrease in overtime
- 30–40% cost savings
What’s the True Financial Cost of Doing Nothing?
Here’s the business case your CFO wants:
- Turnover cost per RN: $61,110 per departure (NSI).
- Hospitals lose $3.9M+ annually due to turnover.
- Revenue cycle disruptions from coding shortages cost:
- Delayed reimbursement
- Increased DNFB
- Slower AR resolution
- Audit exposure
- Lower quality scores
For coding specifically:
- Each vacant coder role can impact $1M+ annually in downstream cash flow.
What Should You Do Next as an HIM or Revenue Cycle Leader?
Here’s your immediate retention blueprint:
- Conduct stay interviews this month. Ask coders: “What makes you want to stay? What might make you leave?”
- Implement flexible scheduling within 30 days.
- Launch recognition rituals. Example: “Weekly Wins” celebrating coding accuracy, productivity, or audit success.
- Build a development pathway. Documented tracks higher morale and longer retention.
- Consider a hybrid outsourcing model to stabilize workloads.
- Benchmark compensation annually not every 3 years.
- Improve communication transparency. Clarity reduces burnout.



How Do You Retain Coding Talent in 2025 and Beyond?
The 31% “intent to leave” statistic is a wake-up call not just for nurses, but for every HIM and revenue cycle leader responsible for coding operations. The factors driving staff out of healthcare burnout, inflexible schedules, lack of recognition, and insufficient career development are completely solvable with the right strategies.
Your coding teams are the backbone of your revenue cycle.
Keeping them supported, engaged, and empowered is no longer optional.
It’s a leadership mandate.
FAQs
What factors are driving medical coders to consider leaving their jobs?
Factors include burnout from rising denials/complexity, stagnant salaries amid 11% market pressure, lack of remote flexibility (86% retention factor), limited career growth, alert fatigue, poor recognition.
How do coding staffing shortages impact revenue cycle performance?
Shortages cause claim backlogs, increased denials (11-20%), coding errors, delayed reimbursements, higher A/R days, quality score impacts from incomplete documentation.
What retention strategies have proven effective in healthcare systems?
Structured recognition (36% turnover reduction via platforms), remote/flexible work, strategic compensation, career upskilling tracks, well-being programs (VR/rest spaces).
How can organizations reduce coder burnout and turnover?
Monthly recognition touchpoints, flexible schedules (86% stay factor), Employee Well-being Centers, celebrate accuracy/TAT milestones, reduce alert fatigue via prioritization.
What role does training and career advancement play in coder retention?
Critical; 75% HIM pros need upskilling for AI/EHR changes; micro-promotion tracks (junior→senior→specialty), apprentice programs boost retention 36%.
How can automation be used without disrupting coder engagement?
Position as workload relief (CAC/AI coding), upskill for oversight roles, maintain human validation loops, focus coders on complex cases vs. repetitive tasks.
What metrics should coding leaders track to anticipate attrition?
Turnover rates, query response times, productivity drops, engagement scores, exit interview themes, vacancy duration, overtime hours signaling burnout.
How are flexible work models affecting coder retention?
Remote work now expectation; 86% cite flexibility as top retention reason per McKinsey; hybrid models with shift flexibility reduce turnover significantly.
How does compensation and benefits competitiveness impact coding talent?
Competitive pay + culture retains at 11% lower cost (NSI); retention bonuses, comprehensive benefits counter national salary pressures from urban/rural competition.
What is the business cost of a high coder turnover rate?
Recruitment/training ($25K+ per coder), denial rework ($25-$118/claim), 65% claims never resubmitted, backlog delays, quality score penalties.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.
