10 CDI Leaders Share Best Practices for Concurrent Review Implementation
Why Concurrent Review Implementation is Crucial?
Concurrent Review has become one of the most critical levers for strengthening Clinical Documentation Integrity (CDI) programs in 2026. As payer scrutiny intensifies, denial rates rise, and quality outcomes directly influence reimbursement, CDI leaders like you, HIM Directors, CDI Directors, and VPs of Revenue Cycle, are asking one core question:
What are the best practices for implementing Concurrent Review that actually improve documentation quality, reduce denials, and elevate patient outcomes?
To answer this directly, we gathered insights from 10 respected CDI directors and industry experts, each offering practical guidance you can apply immediately. Their quotes highlight what’s changing in 2026 and how top-performing organizations are adapting.
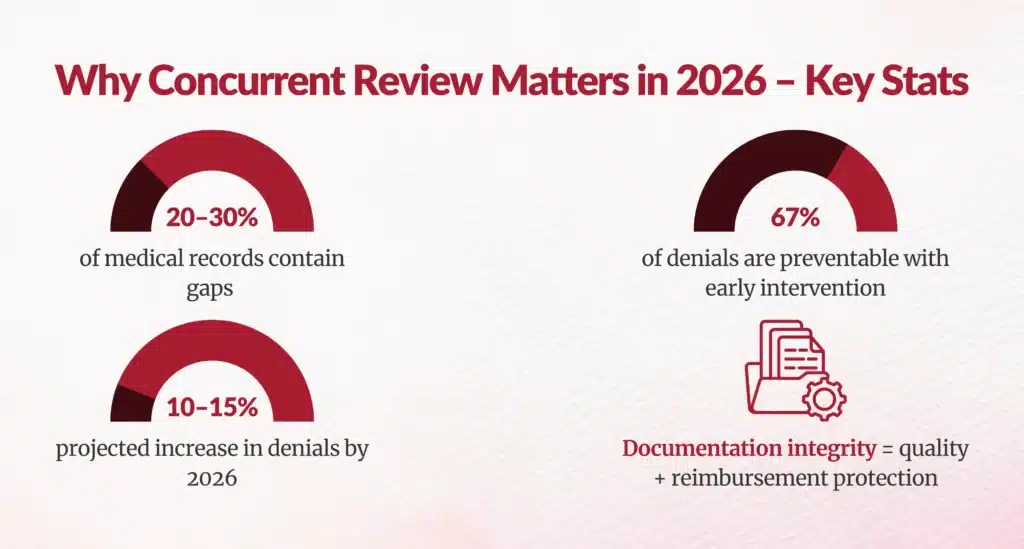
According to AHIMA, 20–30% of medical records contain documentation gaps that impact quality scores and reimbursement (AHIMA) and nearly 67% of denials are preventable with early documentation intervention. These statistics reinforce why concurrent review is no longer optional, it is foundational.
This expert roundup addresses the strategic shift happening across CDI: from code chasing to quality-driven, outcomes-focused, denial-preventive documentation excellence.
What Is the New Strategic Focus of Concurrent Review in 2026?
Whether your organization operates in a Fee-for-Service (FFS) environment or relies heavily on DRG-based reimbursement, Concurrent Review plays a foundational role in capturing the clinical truth while the patient is in-house.
For FFS, real-time documentation accuracy affects medical necessity validation, charge capture, and audit defensibility.
For DRG-driven systems, concurrent CDI directly influences SOI/ROM, DRG assignment, MCC/CC capture, and downstream denials prevention.
This article is intentionally structured to support leaders operating in both FFS and DRG models, since concurrent review strengthens documentation integrity across all reimbursement frameworks.
Why are CDI leaders shifting from reimbursement-only to quality-driven documentation?
Many CDI executives agree that the biggest transformation is not technological, it’s philosophical. Concurrent Review is evolving from a transactional audit function into a strategic driver of documentation accuracy, risk adjustment, and care quality.
“Physician engagement at Novant Health remains strong; leadership recognizes our CDI program’s positive impact on the organization and patient outcomes.”
– Rebecca Truett, RN, MSN, MBA, CCDS, CDI specialist, Novant Health
Source: ACDIS article
This mirrors what many CDI leaders are doing today: moving beyond review counts and query volume, and focusing on metrics tied to severity capture, risk adjustment, and quality outcomes.
“Hospitals are now evaluated just as much on quality outcomes as on reimbursement performance. Our concurrent review strategy ensures documentation fully reflects acuity, clinical intent, and care complexity at the point of service, whether we’re focused on DRG accuracy or supporting medical necessity in FFS environments.”
– Erica Thompson, RN, CCDS, Director of CDI, Northwestern Memorial Hospital
How this helps your organization:
- Aligns CDI impact with enterprise strategic goals
- Helps HIM leaders demonstrate ROI beyond financial metrics
- Reduces coding variability through consistent documentation behavior
- Prepares providers for quality-focused risk adjustment models
How Can Concurrent Review Strengthen Documentation Accuracy and Physician Engagement?
What role does real-time physician support play?
Modern CDI programs are shifting away from retrospective querying to real-time nudging and education.
“Concurrent review allows CDI specialists to address documentation needs while physicians are still actively managing the case. Real-time clarification prevents retrospection delays, improves SOI/ROM, and supports both DRG accuracy and medical necessity documentation for FFS claims.”
– James Holloway, MHA, RHIA, System Director of Clinical Documentation, Indiana University Health
“Quotas don’t support meaningful CDI work.”
– Amy Campbell, Lifepoint Health
“Personally, I am not a fan of review quotas… Our job is to support providers by surfacing accurate information at the point of care.”
Campbell stresses that CDI must shift from volume-driven behavior to value-driven chart analysis.
What this means for leaders like you:
- Build CDI workflows around clinical indicators, not quotas
- Use concurrent review to spark provider trust, not frustration
- Improve both documentation completeness and physician satisfaction
How Are CDI Leaders Using Concurrent Review to Reduce Denials?
Denials are rising. Medicare Advantage plans now deny claims at rates nearly double traditional Medicare (KFF). The earlier documentation gaps are caught, the fewer downstream appeals you face.
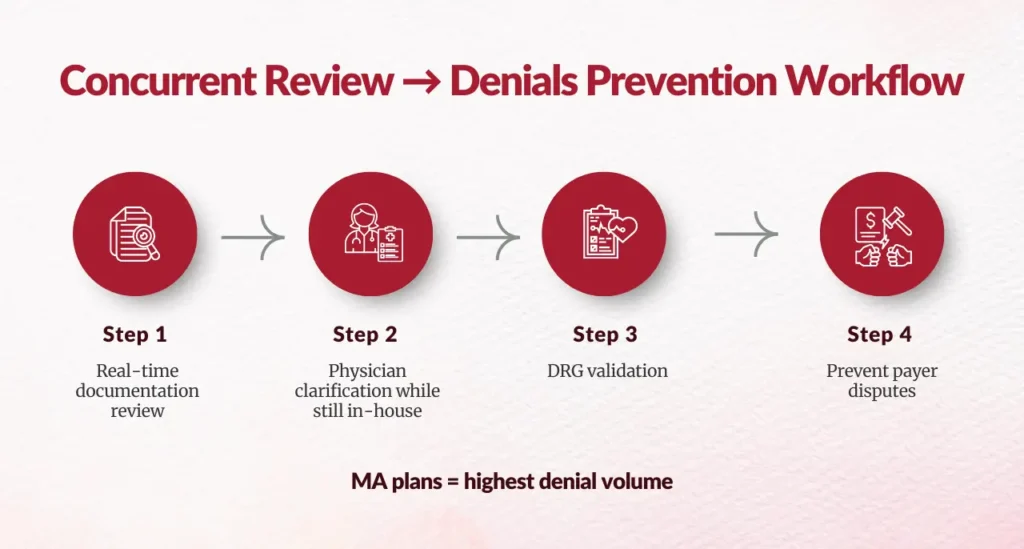
How does CDI strengthen DRG validation and prevent payer disputes?
“CDI must play a larger role in DRG validation.”
-Payal Sinha, Montefiore
“As payers increase scrutiny… organizations are recognizing the value of CDI expertise.”
Sinha notes that CDI involvement earlier in the encounter helps ensure DRG accuracy before claim submission.
We have a sepsis task force at Mercy that educates providers not just to prevent a denial, but to improve preventative and patient care.”
– Mary Bourland, DNP, RN, VP of Coding, CDI and Utilization Management, Mercy Health
Source: Solventum
Multiple studies show Medicare Advantage denial rates and chart reviews climbing faster than traditional Medicare, especially around DRG downgrades and “medical necessity” disputes.
How this helps organizations:
- Reduces costly downstream appeals
- Strengthens audit-readiness
- Improves DRG accuracy and compliance
- Ensures alignment between clinical truth and coding

How Concurrent Review Reduces Denials
How Should Concurrent Review Be Tailored for Specialized Populations?
Why do pediatric and critical-care settings benefit from a tailored CDI approach?
“The pediatric population is not just little adults, not clinically and not when it comes to CDI and coding.“
Brian Murphy, Norwood, referencing pediatric CDI
Source: Norwood article
Pediatric leaders consistently point out that NICU and PICU documentation requires far greater precision than typical adult medical-surgical units, because the acuity, procedures, and DRG behavior are so different.
What Leadership Practices Enable Successful Concurrent Review Programs?
What does effective team engagement look like in CDI?
“CDI teams start to feel more like they are an extension of the care team.”
Kearstin Jorgenson, MSM, CPC, COC, Operations Director, Intermountain Health
Source: Solventum
Strong CDI programs are built on:
- Transparent communication
- Multidisciplinary collaboration
- Continuous education
- Emotional safety to raise concerns
How can CDI teams stay future-ready?
“Early adoption of advanced workflows is critical.”
Lori Dixon, Piedmont Healthcare
“We believed in looking to the future…”
Dixon explains that early adoption of prioritization tools, automated workflows, and AI-supported review methods positioned her organization to handle growing case complexity.
What Are the Key Takeaways for CDI and HIM Leaders Implementing Concurrent Review in 2026?
What Should You Prioritize Right Now?
Based on expert insights, here are the five immediate priorities:
- Shift CDI focus from reimbursement to quality & outcomes
- Adopt real-time physician engagement tools
- Integrate CDI into denials prevention workflows
- Tailor concurrent review processes to specialized units
- Build a culture of collaboration and provider trust
Why Does This Matter for Your Health System?
- Denials will increase by another 10–15% in 2026
- Risk adjustment accuracy now directly influences reimbursement
- Payer audits are becoming more aggressive
- Documentation is foundational to patient care quality, safety, and equity
Concurrent Review is the mechanism that ensures the clinical truth, as Dr. Cesar Limjoco describes it, is captured in the record the first time, not after discharge, not during an audit, and not during an appeal.


How Can Your CDI Program Level Up in 2026?
If you’re a CDI Director or HIM leader aiming to elevate documentation quality while safeguarding reimbursement, the path is clear:
Concurrent Review is no longer a workflow; it is a strategic priority.
The insights shared by 10 respected CDI leaders reinforce that real-time documentation integrity enables:
- More compliant coding
- Stronger payer defensibility
- Improved quality scores
- Better patient outcomes
- Greater provider alignment
The organizations that embed CDI into daily clinical decision-making rather than treating it as an administrative afterthought will lead the industry in accuracy, sustainability, and financial resilience.
FAQs
What exactly is concurrent review in CDI, and why does it matter?
Concurrent review evaluates clinical documentation and coding accuracy during active patient care before claim submission, preventing 67% of denials through real-time gap closure and SOI/ROM accuracy.
What are the first steps to implementing a successful concurrent review program?
Secure executive buy-in, assess current workflows/gaps, pilot small high-impact units, integrate CDI-coder-provider communication channels, establish baseline metrics.
How should CDI teams choose chart triggers and prioritization criteria?
Prioritize high-acuity cases, DRG variance potential, known documentation gaps, physician outliers; use AI/NLP screening for efficiency targeting 70-80% penetration.
What best practices improve provider engagement with concurrent review?
Real-time verbal clarifications over written queries, physician education on DRG/quality impact, peer champions, celebrate accuracy milestones, reduce query volume.
What technology and tools support efficient concurrent review workflows?
Real-time EMR access, NLP gap detection, AI chart prioritization, mobile query apps, integrated dashboards for CDI-coder-provider collaboration.
What performance metrics indicate concurrent review success?
CMI stability/growth, query response rates >85%, denial overturn rates, DRG shift impact, documentation gap closure rates, provider agreement rates.
How can CDI leaders address resistance to change during implementation?
Position as clinical quality partner not revenue chaser, demonstrate financial/clinical wins, start voluntary pilots, leadership visibility, feedback loops.
What governance structure ensures concurrent review sustainability?
Executive steering committees, KPI dashboards, annual audits, cross-department charters defining roles, continuous training refreshers.
How do CDI leaders measure the financial impact of concurrent review?
Track CMI gains, denial reductions (pre/post), DRG reimbursement uplift, rework savings, query ROI through financial modeling.
What common mistakes should organizations avoid in concurrent review rollout?
Over-querying providers, ignoring coder integration, lacking technology support, poor metric selection, scaling before pilot validation.
Author Bio:

Kanar Kokoy
CEO - Chirok Health
Healthcare CEO & CDI/RCM innovator. I help orgs boost accuracy, integrity & revenue via truthful clinical docs. Led transformations in CDI, coding, AI solutions, audits & VBC for health systems, ACOs & more. Let’s connect to modernize workflows.
